Systemwide Limb Salvage Advisory Council Launched
November 24, 2019
Novel multidisciplinary activations are preventing amputation
Innovations in Cardiovascular Medicine & Surgery | Fall 2019
 Mehdi H. Shishehbor, DO, PhD, MPH
Mehdi H. Shishehbor, DO, PhD, MPHFew life events are more physically and psychologically traumatizing than amputation. That’s why University Hospitals Cleveland Medical Center physicians are steadfast in their commitment to explore every option prior to removing a patient’s limb. This past spring, the Limb Salvage Advisory Council (LSAC) launched systemwide, bringing together experts to consult and collaborate in “no option” cases of advanced peripheral artery disease (PAD) or critical limb ischemia (CLI).
“What we have learned nationally is that many patients undergo major amputation without any significant vascular evaluation,” says Mehdi H. Shishehbor, DO, PhD, MPH, Director, Interventional Cardiovascular Center, and Co-Director, Vascular Center, University Hospitals Harrington Heart & Vascular Institute; Clinical Assistant Professor of Medicine, Case Western Reserve University School of Medicine. “Our commitment is that no patient in our system, across 10 hospitals, will undergo an above- or below-the-knee amputation without a full evaluation by our multidisciplinary LSAC team.”
Early results have been dramatic: Of the 21 initial cases presented, the LSAC team strategized innovative care plans to prevent amputation for 17 patients. “These are people who are essentially scheduled for amputation just prior to LSAC consult,” says Dr. Shishehbor. “Even if you save one of them, you are saving a leg.”
 UH Limb Salvage Advisory Team.
UH Limb Salvage Advisory Team.PREVENTING AN AMPUTATION
In fact, a recent successful case involved a 38-year-old woman who had stents placed at an outside hospital for severe leg pain. Unfortunately, the stents clotted, so she turned to UH Cleveland Medical Center for further evaluation. When multiple operations failed to restore sufficient blood flow, she was scheduled for an above-the-knee amputation.
“Under our new protocols, this patient was brought to the attention of the LSAC council. After her case was discussed by the interdisciplinary team, it was decided that maybe we could offer her advanced revascularization,” says Dr. Shishehbor. “In a series of two procedures, we were able to traverse the many blockages to restore blood flow and save her leg.”
Through a combination of highly complex endovascular procedures and clot-dissolving medication therapy, Dr. Shishehbor was able to reconstruct many of the arteries that sustained damage during the prior six months and return sufficient perfusion to the foot. Now, instead of learning to stand on one leg, this patient is walking pain free because of the commitment of LSAC team members to exhaust every medical option before amputation occurs.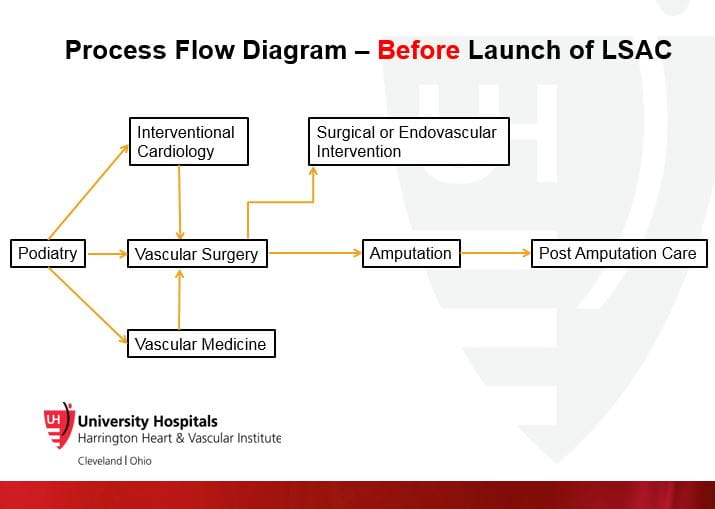
SEAMLESS CONNECTIVITY
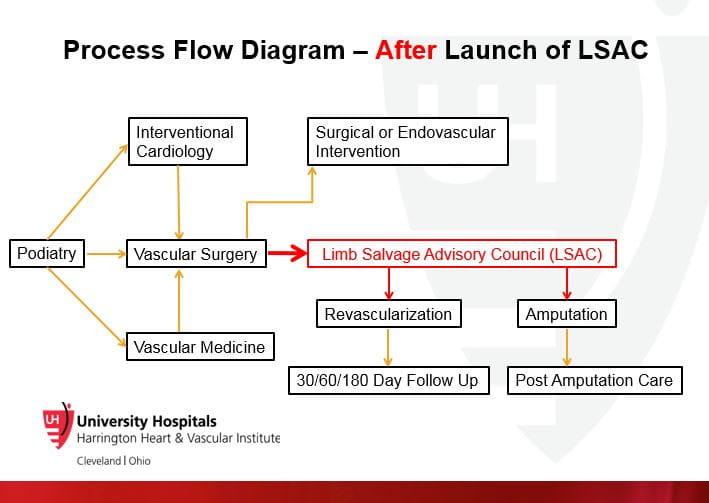
Each LSAC activation connects a multidisciplinary team via secure Cisco Webex videoconferencing, including as indicated:
- interventional cardiology
- nutrition
- pain management
- plastic surgery
- podiatry
- prosthetics
- vascular medicine
- vascular surgery
- wound care
Participants log in remotely to hear case presentations and visualize on-screen patient data, including histories, angiograms, arterial duplex, X-rays and wound images. “We wanted the advisory council to be nimble and efficient,” says Dr. Shishehbor. “Our experts can be anywhere in the world and be able to review and comment on the case being presented.”
LSAC activations follow a multidimensional algorithm. It defines the relevant components of each case as participants work in concert to strategize novel surgical or vascular options, request additional scans or tests and determine if the patient is a candidate for specialized treatments such as hyperbaric therapy, stem cells or regional anesthetic modalities.
HOLISTIC APPROACH BENEFITS
In addition to limb salvage, the unique LSAC concept is serving to highlight excellence and standardize care throughout the system. “Not everybody has the same skill sets or techniques,” says Dr. Shishehbor. “LSAC collaborations enable us to share our expertise and ensure each patient is getting appropriate, advanced care.” That includes revascularization techniques and supportive care necessary to prevent future risk of wounds, ulcers and gangrene.
Patients with advanced PAD or CLI often present with complex challenges such as uncontrolled diabetes or renal failure, making them difficult surgical candidates. Even when patent vascular interventions provide adequate blood flow, persistent wounds often fail to heal. By fostering a holistic approach and connecting patients to appropriate medical therapies, LSAC is providing new hope for these patients who had nowhere to turn.
Contact Dr. Mehdi Shishehbor at 216-553-1439.