Breaking the Silence: Understanding Diabetes-Related Depression
March 11, 2024
Innovations in Diabetes & Metabolic Care | Winter 2024
As prevalence of Type 1 and Type 2 diabetes mellitus (T1/T2DM) increases across the United States, there is a concerning coexistence of depressive symptomology. According to original research recently posted by the Centers for Disease Control and Prevention (CDC), data gathered from the Behavioral Risk Factor Surveillance System from 2011 to 2019 showed that one in nine U.S. adults had a diagnosis of diabetes, and one in five had a diagnosis of depression.1
 Betul Hatipoglu, MD
Betul Hatipoglu, MDAdditionally, the study’s authors found “[t]he prevalence of depression was consistently more than 10 percentage points higher among adults with diabetes than those without diabetes.”2
“Depression is the elephant in the room that we need to acknowledge in people with diabetes,” says Betul Hatipoglu, MD, Medical Director of the Diabetes and Metabolic Care Center and the Mary B. Lee Chair in Adult Endocrinology at University Hospitals Cleveland Medical Center. “Unless we recognize depression and share with our patients that it may be a significant component of their disease manifestation, we will fail over and over in helping them make impactful, holistic choices to develop healthy lifestyles.”
Dr. Hatipoglu prioritizes recognizing and addressing clues of depression or despair in her patients. “When glucose levels are suddenly higher in a patient that otherwise was stable, that is alarming,” she says. “So often, when I see patients turning to food for comfort, stopping medications or losing interest in blood sugar monitoring, these are reactive findings that reveal an emotional struggle.”
Preventing an Unhealthy Cycle
When depression is unchecked, a downward spiral can occur. “Where there are feelings of depression or fatigue, individuals lack motivation to manage their diabetes,” Dr. Hatipoglu says. “For example, they may withdraw from exercise and healthy eating, which affects blood sugar and medication compliance.” Fortunately, with appropriate diabetes and mental healthcare, individuals can reverse the spiral.
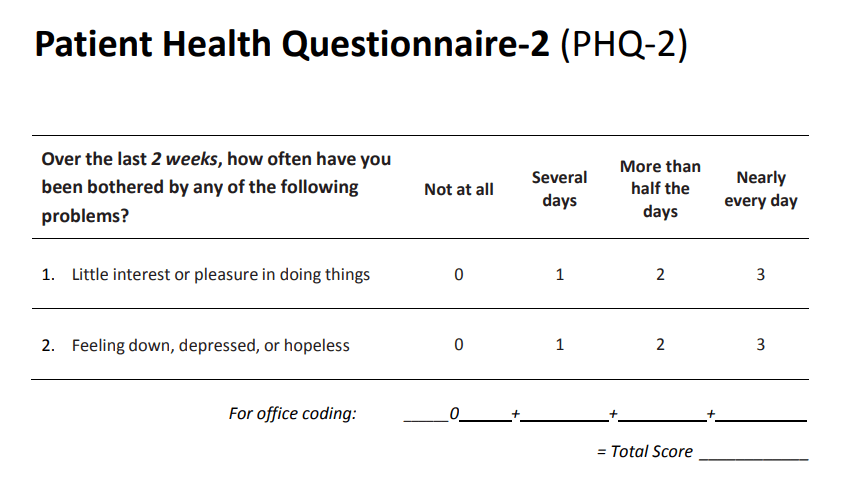
Dr. Hatipoglu highlights the need for endocrinologists, diabetes specialists and primary care providers to incorporate validated mental health screening tools into routine patient appointments. Something as simple as the Patient Health Questionnaire (PHQ) can help flag depression before it becomes debilitating. The PHQ-2 is the first two questions of the PHQ-9, and a score of 3 or more indicates likely depressive disorder, highlighting the need for providers to offer treatment resources. Available in more than 30 languages, the PHQ-2 is free and easy to administer.
“When we treat a disease that has been affecting someone’s life, the scientific medical community has historically been trained to think that if we write prescriptions and recommend lifestyle changes, everything will be fine,” Dr. Hatipoglu says. “When everything isn’t fine, it is too often seen as the patient’s fault.”
When Dr. Hatipoglu identifies depression or anxiety in her patients, she will offer a medication — typically escitalopram (Lexapro) or sertraline (Zoloft) — to lessen symptoms until the individual can seek care from a psychiatrist or psychologist.
“Sometimes individuals are so overwhelmed with chronic illness and life challenges such as stressful work or taking care of family that they are taxing neurotransmitters in the brain,” she says. “Like a vitamin D deficiency that needs replenishment, medications might be needed to reestablish those neurotransmitters and empower mental wellbeing.” Dr. Hatipoglu also stresses that studies show infusing complementary modalities into treatment plans, including yoga, meditation, light therapy or walking in nature, can help reverse depression in selected individuals.
A Paradigm Shift
“We often have the cognition of what it takes to be healthy, but we need to infuse that nebulous knowledge into what I call body empowerment,” Dr. Hatipoglu says. “When there is wholeness in the healing process, individuals living with diabetes can prevent further advancement or even reverse the disease.”
For more information about the link between diabetes and depression, contact Betul Hatipoglu, MD, at Betul.Hatipoglu@UHhospitals.org.
1,2 Koyama AK, Hora IA, Bullard KM, Benoit SR, Tang S, Cho P. State-Specific Prevalence of Depression Among Adults With and Without Diabetes — United States, 2011–2019. Prev Chronic Dis 2023;20:220407. DOI: http://dx.doi.org/10.5888/pcd20.220407
Contributing Expert:
Betul Hatipoglu, MD
Medical Director
Diabetes and Metabolic Care Center
Vice Chair, UH System Clinical Affairs
Mary B. Lee Chair in Adult Endocrinology
University Hospitals Cleveland Medical Center
Professor
Case Western Reserve University School of Medicine


