University Hospitals Vascular Surgeon Bolsters Case for Evaluating European Dissection Specific Stent Graft
December 06, 2023
Research shows differences in wall shear stress created by the novel device design crucial explanatory factor in better patient outcomes
Innovations in Cardiovascular Medicine & Surgery | Fall 2023
A vascular surgeon from University Hospitals Harrington Heart & Vascular Institute has led an international research effort to explain one key factor behind the success of a novel dissection-specific stent graft being used at select centers in Europe.
 William Yoon, MD
William Yoon, MDWilliam Yoon, MD, Co-Director of the Aortic Disease Center at UH Harrington Heart & Vascular Institute, and colleagues from Sweden, created computer models of fluid dynamics using data from 14 European patients with chronic type B aortic dissection who received the dissection-specific stent graft, as well as three patients who received the standard thoracic graft. Their analysis shows that differences in wall shear stress created by the different device designs is a crucial explanatory factor in patient outcome. Results were published in the European Journal of Vascular & Endovascular Surgery.
“Being geometrically enhanced with reduced radial force, the dissection-specific stent graft induces changes in shear stress distribution different from those with standard stent grafts, transitioning high wall shear stress zones into the stent-covered aorta,” Dr. Yoon says.
This transition, he says, may help prevent intimal injury and consequent development of distal stent graft-induced new entry (dSINE) – a growing problem in vascular surgery.
“A major challenge in treating aortic dissection is unsatisfactory compliance of the distal portion of stent grafts in a dissected aorta,” he says. “With type B dissections, there is a septum in the aorta between the true aortic lumen and the false lumen in the middle aortic wall layer created by aortic wall dissection (tear). The stent graft is placed into the true lumen, but the stent graft, because it has its own expanding radial force, can tear the septum – sometimes after some time, sometimes right away. When this happens, it can create a new tear which can lead to false lumen pressurization and expansion with rupture risk.”
The design of the European dissection-specific stent graft addresses these challenges, Dr. Yoon says. It offers customization of diameters and lengths with substantial tapers, allowing it to be individualized to the patient. Its second and third Z stents have reduced radial force compared with standard thoracic stent grafts. Importantly, its most distal stent is removed, leaving instead a small measure of unsupported Dacron fabric known as the “endovascular elephant trunk.”
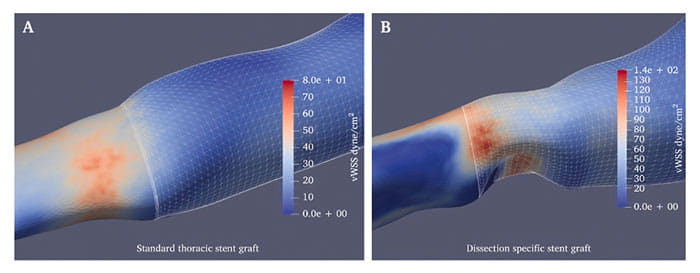 Figure 1: Wall shear stress (WSS) distribution map of standard thoracic stent graft (A) and of dissection specific stent graft (B), showing differences in the occurrence site of high WSS regions: uncovered native segment of the aorta (distal to the stent graft) in the standard thoracic stent graft cases vs. covered segment of the aorta in the dissection specific stent graft cases (inside the stent graft).
Figure 1: Wall shear stress (WSS) distribution map of standard thoracic stent graft (A) and of dissection specific stent graft (B), showing differences in the occurrence site of high WSS regions: uncovered native segment of the aorta (distal to the stent graft) in the standard thoracic stent graft cases vs. covered segment of the aorta in the dissection specific stent graft cases (inside the stent graft).© 2023 The Authors. Published by Elsevier B.V. on behalf of European Society for Vascular Surgery.
“As a result, only the dissection-specific stent graft fabric is in direct contact with the inner aortic wall at the distal part of the graft,” he says. “All these features, while restricting the radial outward force at the distal end, contribute to the enhanced flexibility and conformability of the dissection-specific stent graft, thereby improving its compliance compared with the standard thoracic model.”
In fact, among the 16 type B dissection patients whose data formed the basis of the research team’s computer model, Dr. Yoon and his colleagues found rates of dSINE of just 6 percent in those with the novel stent – compared with up to 28 percent among those with the standard thoracic stent graft.
Dr. Yoon says he hopes this work and the growing problem of dSINE – which the European graft reduces – will speed the process of launching clinical trials of the dissection-specific stent graft in the United States. The process of evaluating and approving medical devices, in particular, is unacceptably slow, he says.
“As we get more evidence for it, we could make an argument for in potential clinical trials in the United States,” he says.
There are patients who could clearly benefit, especially those at high risk of dSINE.
“These include patients with a narrow true lumen of the distal landing zone, documented
connective tissue disorder and a history of dSINE from a previous procedure,” Dr. Yoon says. “The clinical need is clear.”
For more information, contact Dr. Yoon’s office at 216-844-3013.
Contributing Expert:
William Yoon, MD
Co-Director, Aortic Disease Center
University Hospitals Harrington Heart & Vascular Institute
Associate Professor
Case Western Reserve University School of Medicine


