Novel Cardiac MRI Protocol Explores Impact of COVID-19-Linked Myocardial Injury
October 21, 2020
New approach captures a highly detailed assessment of heart and lung function in a subset of survivors
Innovations in Cardiovascular Medicine & Surgery | Fall 2020
 Sadeer Al-Kindi, MD
Sadeer Al-Kindi, MDA study funded by University Hospitals Cleveland Medical Center is underway to investigate the extent of heart and lung damage in a subset of COVID-19 survivors. Utilizing an integrated cardiopulmonary exercise cardiac MRI protocol, internationally recognized cardiology specialists within University Hospitals Harrington Heart & Vascular Institute in Cleveland, Ohio, are capturing a highly detailed assessment of heart and lung function.
“In a percentage of patients hospitalized with COVID-19, we noticed evidence of heart damage without obvious reasons for preexisting heart disease,” says Sadeer Al-Kindi, MD, a cardiologist at UH Harrington Heart & Vascular Institute who specializes in advanced cardiovascular imaging.
“These findings have prompted us to study the prevalence and impact of heart abnormalities in survivors,” adds Dr. Al-Kindi, who is also an Assistant Professor at Case Western Reserve University School of Medicine.
The study team includes:
- Dr. Al-Kindi (Principal Investigator)
- Sanjay Rajagopalan, MD, Chief, Division of Cardiovascular Medicine, UH Harrington Heart & Vascular Institute; Herman K. Hellerstein MD Professor of Medicine and Radiology, and Director, Cardiovascular Research Institute at Case Western Reserve University School of Medicine (Co-Principal Investigator)
- David Zidar, MD, PhD, cardiologist at UH Harrington Heart & Vascular Institute and an Associate Professor at Case Western Reserve University School of Medicine (Co-Investigator)
A GLOBAL CONCERN
Early international findings document cardiac injury in one out of four patients hospitalized with COVID-191, and the virus may be associated with cardiac dysfunction, arrhythmia, inflammation and fibrosis. Even after fever and common symptoms subside, a significant number of patients struggle with lingering shortness of breath and exercise intolerance.
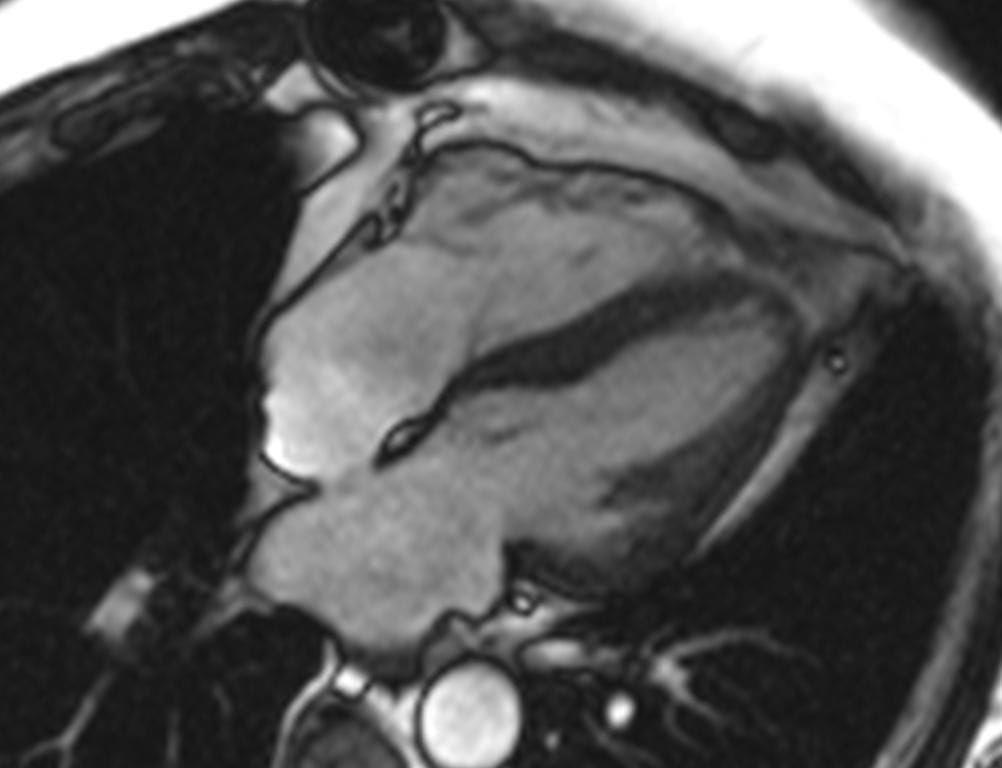 Cardiac MR image.
Cardiac MR image.As an alarming number of previously healthy individuals with a mild to moderate COVID-19 symptom burden progress to myocardial injury, researchers around the world are racing to find answers:
- What is the prevalence of myocardial injury and arrhythmia in COVID-19 survivors?
- What role does inflammatory response play?
- How do the heart and lung respond to available treatments?
- How does COVID-19-linked myocarditis respond as compared to other causes of cardiac inflammation?
- What best practices protocols should be established to improve outcomes for COVID-19 survivors?
The year-long UH study will recruit 50 COVID-19 patients with prior non-ICU hospitalization who have symptom resolution and are at least two weeks past presumed recovery. The experimental group will consist of 25 adults who had inpatient elevated troponin (three times the upper limit of normal). The control group will consist of age- and sex-matched peers who had normal inpatient troponin levels.
“The pandemic has provided an unprecedented model to study associations between myocardial injury and cardiopulmonary function,” Dr. Al-Kindi says. “Using a complex, graded protocol, we are investigating the heart and its correlates for evidence of lasting myocardial damage.”
ADVANCED IMAGING CAPABILITIES
Sophisticated imaging, combined with exercise physiology and analysis of inflammation, will extend the understanding of persistent myocardial fibrosis and edema and the activation of fibrotic and inflammatory pathways. The trial will utilize cardiovascular MRI to characterize the myocardium and define edema and diffuse fibrosis.
After initial resting imaging is completed, patients will engage in an integrated cardiopulmonary exercise test that incorporates a recumbent bicycle. At peak exercise, patients will go back to the scanner for additional imaging to assess cardiac volume and flow. “We hope to better understand to what extent residual shortness of breath and decreased myocardial reserve correlate with exercise intolerance and ongoing cardiopulmonary dysfunction,” Dr. Al-Kindi says.
The pioneering approach, initially implemented by UH experts to study heart failure, will track dynamic changes while providing simultaneous myocardial mapping. “The cardiopulmonary test gives us a tremendous amount of information about both heart and lung status,” Dr. Rajagopalan says. “Very few hospitals around the world are able to perform this advanced level of cardiopulmonary exercise testing.”
Additionally, study data gathered in the health system’s COVID-19 registry will provide a storehouse for impactful ongoing cardiopulmonary research.
For more information, call 216-368-6895 or email Dr. Al-Kindi at Sadeer.Al-Kindi@UHhospitals.org.
1 Guo T, Fan Y, Chen M, et al. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease. 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811–818. doi:10.1001/jamacardio.2020.1017


