UH Rainbow's Fetal Cardiac Intervention Program
November 17, 2019

Improving outcomes for high-risk fetal heart defects
Innovations in Congenital Heart - Fall 2019
 James Strainic, MD
James Strainic, MDFrom the first ultrasound, parents are eager for confirmation that their unborn child is healthy and developing soundly. If an abnormality is detected, panic can set in. Fortunately, parents have a place to turn when a fetal heart problem is discovered.
The Fetal Cardiac Intervention Program is part of The Congenital Heart Collaborative, an innovative affiliation among University Hospitals Rainbow Babies & Children’s Hospital, University Hospitals MacDonald Women’s Hospital and Nationwide Children’s Hospital, located in Columbus, Ohio. This collaboration brings together an expert team of highly skilled providers, 24/7 access to seamless care delivery, and novel therapies. The team is the only one in Ohio and one of only eight nationally to offer fetal cardiac intervention. Referrals have come from New York, Pennsylvania and the United Arab Emirates.
UH FETAL HEART PROGRAM
The Fetal Heart Program at UH Rainbow Babies & Children’s Hospital performs more than 800 fetal echocardiograms each year and refers families to the fetal intervention team when indicated. “To date, we have nine maternal-fetal pairs who have undergone fetal cardiac intervention,” says James Strainic, MD, Director of the Fetal Heart Program at UH Rainbow Babies & Children’s Hospital and Assistant Professor at Case Western Reserve University School of Medicine. “The goal of intervention is to favorably alter the progression of heart and lung development so that babies are healthier and more stable at birth, and decrease the number of open heart surgeries they will require in the future.”
Fetal cardiac intervention can occur between 23 and 32 weeks gestation. During the minimally invasive intervention, the mother’s health is paramount. Anesthesia is provided via epidural to the mother, and fetal anesthesia is administered in an arm or leg muscle. The percutaneous transabdominal procedure is performed under ultrasound guidance to access the fetal heart.
Collaboration of the multidisciplinary team is essential, including as needed experts:
- Maternal-fetal medicine (MFM) physicians
- High-risk obstetricians
- Neonatologists
- Pediatric cardiothoracic surgeons
- Pediatric cardiologists and interventional cardiologists
- Multiple pediatric subspecialists
- Maternal and fetal anesthesiologists
- Fetal imaging and echocardiogram technicians
- Geneticists and genetic counselors
- Fetal care navigators and nurse coordinators
- NICU/CTICU
- Social services
- Palliative care
CONDITIONS THAT QUALIFY FOR FETAL INTERVENTION
Impending hypoplastic left heart syndrome with critical aortic stenosis
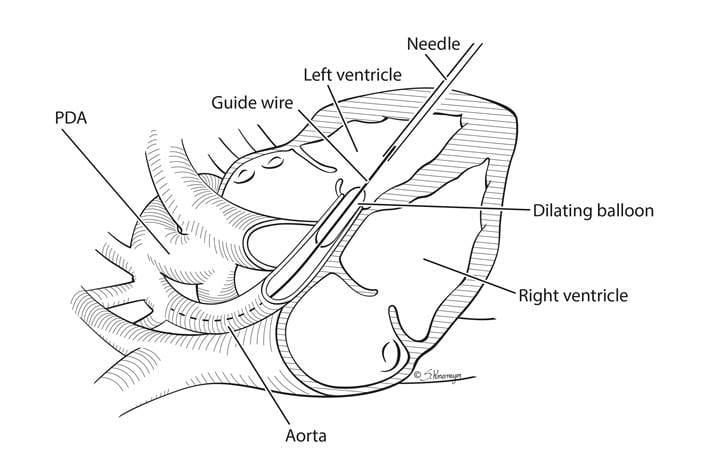 Schematic demonstrating the technique used to open the aortic valve in utero in the setting of severe aortic stenosis and impending HLHS
Schematic demonstrating the technique used to open the aortic valve in utero in the setting of severe aortic stenosis and impending HLHSThese patients have severe blockage of blood flow out of the left pumping chamber, hindering growth of the cardiac muscle. “We intervene to open the aortic valve and encourage blood flow to the pumping chamber,” says Dr. Strainic. “The goal is to provide an increased chance for the left ventricle to grow.”
Ideally, the delicate procedure supports the development of two pumping heart chambers, but in some cases, the left ventricle stops growing despite intervention. Without in utero surgery, the majority of affected babies will have only one pumping chamber and diminished life expectancy.
Read a case study of a successful aortic valvuloplasty performed at 24 weeks gestation.
Hypoplastic left heart syndrome with intact atrial septum
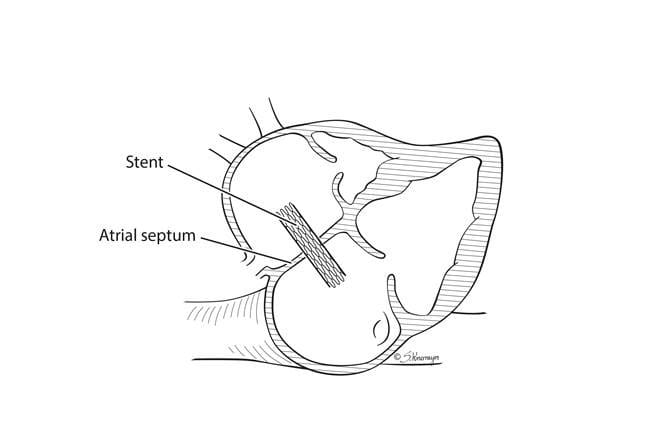 Schematic demonstrating the technique used to place a stent in utero in the setting of hypoplastic left heart syndrome with intact atrial septum.
Schematic demonstrating the technique used to place a stent in utero in the setting of hypoplastic left heart syndrome with intact atrial septum.These patients have already developed a single pumping chamber heart, but they require stent placement to open the wall between the receiving chambers of the heart.
“All fetuses have a naturally occurring hole between the pumping chambers, but it is especially important when you have a single pumping chamber,” says Dr. Strainic. “When the wall is intact, these patients develop high pressure on the left side of the heart, causing high pressure in the pulmonary vein.”
The goal of intervention is to decrease pressure in the left receiving chamber to support normal lung development. Improving blood flow through the pulmonary vessels is critical for lung growth, a key component for the staged surgeries these babies will require in childhood.
“We’ve had a nice success from that procedure, and the baby has undergone his first stage of the palliation for hypoplastic left heart syndrome,” says Dr. Strainic. “Successful fetal intervention is measured through years of monitoring the patient’s condition, but so far, so good.”
Pulmonary atresia with intact ventricular septum and developing hypoplastic right ventricle
In these patients, the pulmonary valve does not form correctly, and the resulting insufficient blood flow causes the right side of the heart to stop developing normally. The muscle thickens because it is subjected to excess pressure, and the right ventricle does not grow well. Successful intervention opens up the valve in utero to encourage blood flow and support heart growth. “We have performed two successful cases, and both babies developed normal-sized right ventricles,” says Dr. Strainic.
The Congenital Heart Collaborative offers 24/7 access. To connect with the Fetal Cardiac Intervention team to discuss a candidate for fetal intervention, please call 216-714-8358 or email Dr. Strainic at peds.innovations@UHhospitals.org.


