LAAC Effective for Patients with HCM and AF New University Hospitals Study Shows
December 06, 2023
Innovations in Cardiovascular Medicine & Surgery | Fall 2023
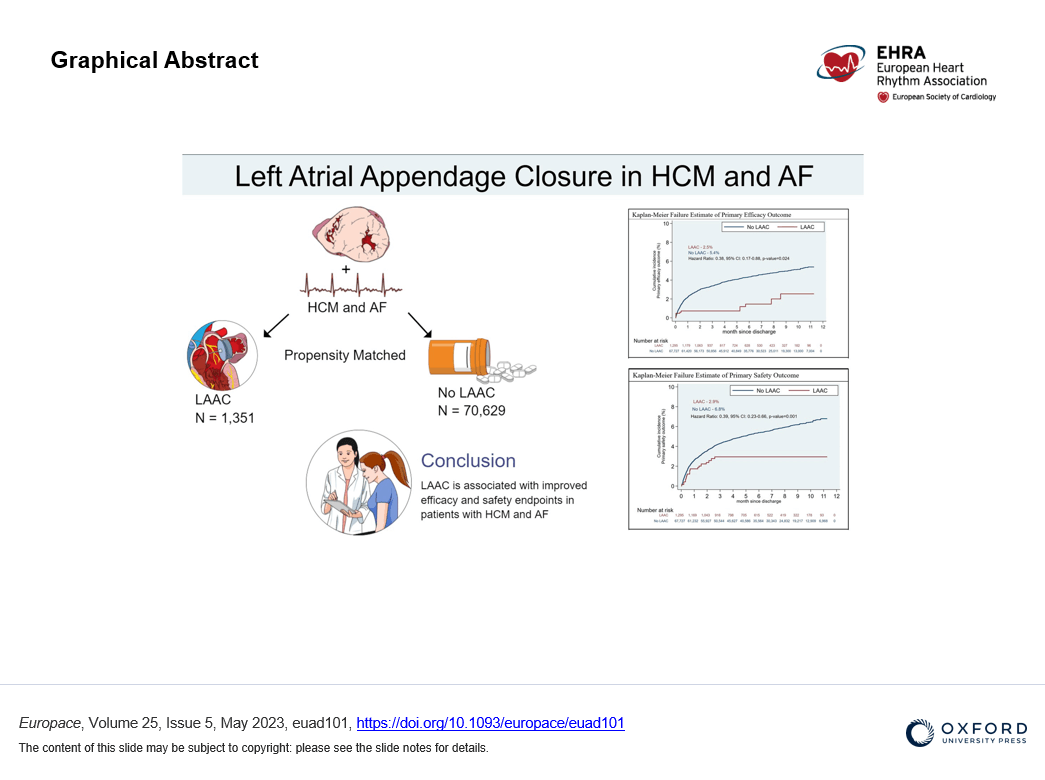
A research team from University Hospitals (UH) Harrington Heart & Vascular Institute has conducted the largest study to date on the benefits of left atrial appendage closure (LAAC) in patients who have both atrial fibrillation (AF) and hypertrophic cardiomyopathy (HCM).
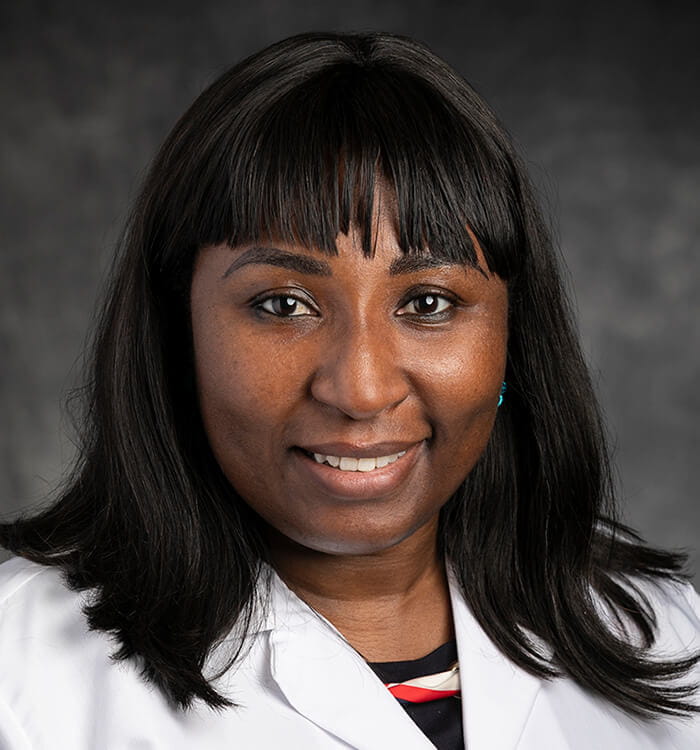 Anene Ukaigwe, MD
Anene Ukaigwe, MDIt’s a special subset of patients with unique needs – and limited research to guide their care when it comes to left atrial appendage occlusion and stroke prevention, says Anene Ukaigwe, MD, an interventional cardiologist at UH Harrington Heart & Vascular Institute and senior author of the new study. Up to this point, robust data on the impact of LAAC on patients with both HCM and AF has been lacking.
“Patients who have HCM represent a special subset,” Dr. Ukaigwe says. “It's a common cardiomyopathy and it’s frequently associated with AF, usually non-valvular AF. There are validated risk scores to predict stroke risk associated with non-valvular AF, like the CHADS2VaSc score, but these don't accurately predict risk in patients who have HCM.”
Given this, the UH team saw an opportunity to help improve care, she says.
“The goal with our study was to see whether LAAC has any benefit in this subgroup of patients,” she says. “Given the high prevalence of AF in HCM patients, the associated high morbidity and mortality and the under-representation of HCM patients in LAAC studies, we sought to use this retrospective cohort to evaluate the efficacy and safety of LAAC in HCM patients with AF.”
Results from the UH team’s retrospective analysis of nearly 72,000 patients diagnosed with both HCM and AF, published in the journal Europace, show that that LAAC does indeed have benefit. They reveal that both surgical and transcatheter LAAC were associated with a lower risk of hemorrhagic stroke and major bleeding among patients with HCM and AF. The risk of all stroke and death was twice as likely in patients who did not have LAAC compared to those who did (5.4% vs 2.5%). At the same time, safety outcomes were also improved. The patients who did not receive LAAC were twice as likely to have major life-threatening bleeding than those who did not (6.8% vs 2.9%).
“With the large cohorts that we had in our study, we’ve demonstrated that with HCM patients with AF stand to benefit from left atrial appendage closure. Dr. Ukaigwe says.
The UH team also found that LAAC patients were likely to be younger, have coagulopathy, obesity and were treated in large hospitals or teaching hospitals. Importantly, they also found that among patients who did not undergo concurrent myectomy for HCM, LAAC still showed efficacy as a treatment.
“This suggests that LAAC is efficacious independent of septal myectomy,” Dr. Ukaigwe says.
The UH team also observed a lower rate of heart failure admissions in the LAAC group, which is counter to previously reported data.
For Dr. Ukaigwe, these results aren’t especially surprising.
“Going into the analysis, I expected LAAC to have some benefits,” she says. “Increasing number of patients who were not tested in the LAAC trial have been demonstrated to have a stroke reduction benefit with LAAC. So our sense was that there will be some benefit. Using the available cohort to validate that was very reassuring.”
Dr. Ukaigwe says next steps for this project include incorporating these promising findings for HCM and AF patients into UH Harrington Heart & Vascular Institute’s innovative HCM Board. This multidisciplinary panel includes specialists in heart failure, electrophysiology, cardiothoracic surgery, cardiovascular imaging, genetics, cardiovascular medicine, interventional cardiology and pediatric cardiology. Questions discussed include a patient’s participation in athletics, the risk of sudden cardiac death and the need for an ICD, and which septal reduction technique is most warranted – surgical myectomy or alcohol ablation. Now there will be more discussion on atrial fibrillation management.
“The next step is to evaluate the impact of LAAC in this subgroup of patients within our institution where we can have where we can get some granularity in the outcomes or benefits, including long-term follow-up,” she says. “Hopefully over time, we’ll be able to form multicenter registries to look at this.”
For now, however, Dr. Ukaigwe’s message to fellow providers is clear.
“The fact that HCM patients were not necessarily included in the trials for LAAC should not preclude them from getting left atrial appendage occlusion when indicated,” she says.
For more information about this study, contact Dr. Ukaigwe at Anene.Ukaigwe@UHhospitals.org.
Contributing Expert:
Anene Ukaigwe, MD
Interventional Cardiologist
University Hospitals Harrington Heart & Vascular Institute


