Two Heart Procedures Recognized with Centers of Excellence Designation
November 10, 2021
Left atrial appendage occlusion and atrial fibrillation ablation offered at University Hospitals Harrington Heart & Vascular Institute receive national recognition
Innovations in Cardiovascular Medicine & Surgery | Fall 2021
Nationally recognized innovations and extraordinary outcomes have led to Centers of Excellence (COE) designations for two procedures offered within the University Hospitals Harrington Heart & Vascular Institute, based at University Hospitals Cleveland Medical Center.
 Mauricio Arruda, MD
Mauricio Arruda, MD Ivan Cakulev, MD
Ivan Cakulev, MD Steven Filby, MD
Steven Filby, MD“With these two percutaneous procedures, atrial fibrillation (AFib) ablation and left atrial appendage occlusion (LAAO), our leadership saw an opportunity to showcase the highly differentiated and frictionless patient experience we are providing and elevate these programs to Centers of Excellence,” says Nate Kunce, MHSA, Business Operations Manager for the Cardiovascular Service Line within University Hospitals Harrington Heart & Vascular Institute. “We have invested in a phenomenal team and infrastructure that hopefully set us apart as the partner of choice within the marketplace for providing optimal value and quality of care.”
COE programs concentrate expertise and resources to deliver high success/low complication rates and cost efficiencies desirable to insurance companies and third-party payers, while fostering an exceptional patient-centered experience.
One unique aspect of the delivery model is proximity. “Our hybrid cath lab and advanced imaging modalities are all within the same shared space,” says Lori Hammer, BSN, RN-BC, Manager of the Valve and Structural Heart Disease Center within University Hospitals Harrington Heart & Vascular Institute. “Our capacity to have patients come in for their pre-planning imaging on the day of their scheduled procedure has been beneficial in eliminating an extra visit, especially for people traveling to us from a long distance.” Same-day services also streamline workflow and reduce overhead as patient volume has increased significantly over the past year.
AFib Ablation Recognized as a Fully Covered Benefit
With high volumes and excellent outcomes, AFib ablation has been officially recognized as a fully covered benefit for the year 2022 University Hospitals employees’ traditional health plan. Mauricio Arruda, MD, Electrophysiologist and Director of the Electrophysiology Center, and Ivan Cakulev, MD, Electrophysiologist, both with University Hospitals Harrington Heart & Vascular Institute, utilize state-of-the-art technologies for mapping and ablation, including a robotic navigation system to offer comprehensive AFib ablation expertise with a 24-hour discharge rate of nearly 95 percent. Another differentiating factor is that, unlike the conventional procedure, their AFib ablation strategy is tailored to each patient presenting to the center.
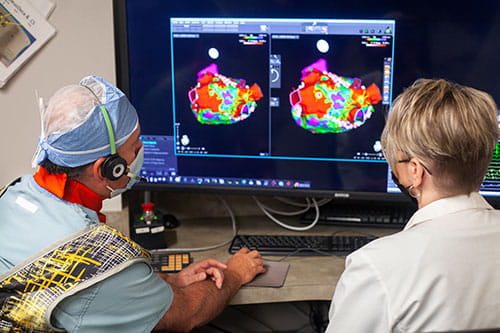
“In many patients, we note that they have developed scattered scar tissue in the left atrium,” Dr. Arruda says. “By ablating this fibrotic substrate in conjunction with pulmonary vein isolation [PVI], patients have a better chance of remaining free from AFib and atrial flutters for a longer period.” Three scientific papers1-3 have recently addressed their techniques.
A New Approach to LAAO
In 2020, LAAO using Watchman™ placement at University Hospitals Harrington Heart & Vascular Institute had a 100 percent success rate, with a device usage rate of 1.0 versus the national average of around 1.4. Several aspects of the procedure set it apart from other institutions.
“We utilize advanced CT scan angiography in place of the more invasive transesophageal echocardiogram for pre-procedural planning, which allows us to have a three-dimensional image of the heart and detailed measurements of the appendage,” says Steven Filby, MD, Interventional Cardiologist and Director of the Cardiac Catheterization Laboratory at University Hospitals Cleveland Medical Center. “The CT scan helps the operator plan with tremendous precision and increases the accuracy of device sizing and placement.”
During the procedures, Dr. Filby and Dr. Arruda utilize intracardiac echo (ICE), a small ultrasound probe placed percutaneously through the groin. These two modalities eliminate the need for general anesthesia. Patients receive conscious sedation, expediting their recovery and enabling 90 percent to go home the same day. This approach has resulted in a 15 percent cost reduction over conventional LAAO, which requires patients to be admitted overnight for observation.
A study recently published in the Journal of Invasive Cardiology4 highlights the team’s advanced methods and favorable outcomes. Additionally, the team is investigating the use of fluoroscopy in LAAO.
“Were taking CT scans of the appendage and overlaying them onto fluoroscopy images,” Dr. Filby says. “The co-registration or fusing of the two studies provides a roadmap of sorts that allows us to identify the exact location of the appendage and accurately place the occluding device.”
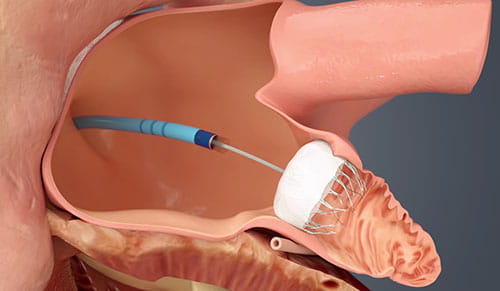 WATCHMAN device.
WATCHMAN device.Research initiatives at University Hospitals Harrington Heart & Vascular Institute are evaluating this novel fusion as a potential matter of protocol and following patients to monitor long-term outcomes. While patients who receive the Watchman device are entered into a national registry, University Hospitals Cleveland Medical Center is also an approved site for the CHAMPION-AF clinical trial aimed at determining if LAAO with the WATCHMAN FLX device is a reasonable alternative to non-vitamin K oral anticoagulants in patients with non-valvular atrial fibrillation.
Industry leaders also rely on University Hospitals Harrington Heart & Vascular Institute expertise to provide early market feedback on new tools, mapping software and devices to test and troubleshoot products before their full market launch. “With everything we do, we try to leverage our knowledge and capabilities to provide the best service to our patients with minimal complications,” Dr. Arruda says.
For more information about the Centers of Excellence procedures or to refer a patient for treatment, please call 216-844-8448.
Contributing Experts:
Mauricio Arruda, MD
Director, Electrophysiology Center and Atrial Fibrillation Center
University Hospitals Harrington Heart & Vascular Institute
Associate Professor
Case Western Reserve University School of Medicine
Ivan Cakulev, MD
Electrophysiologist
University Hospitals Harrington Heart & Vascular Institute
Assistant Professor
Case Western Reserve University School of Medicine
Steven Filby, MD
Director, Cardiac Catheterization Laboratory
University Hospitals Cleveland Medical Center
Assistant Professor
Case Western Reserve University School of Medicine
Lori Hammer, BSN, RN-BC
Manager, Valve and Structural Heart Disease Center
University Hospitals Harrington Heart & Vascular Institute
Nate Kunce, MHSA
Business Operations Manager, Cardiovascular Service Line
University Hospitals Harrington Heart & Vascular Institute
Additionally, an ambulatory order is available through the electronic medical record (EMR) to refer patients to University Hospitals Harrington Heart & Vascular Institute.
References
- Yagishita A, DE Oliveira S, Cakulev I, Gimbel JR, Sparano D, Manyam H, Manrique-Garcia A, Arredondo M, Mackall J, Arruda M. Correlation of Left Atrial Voltage Distribution Between Sinus Rhythm and Atrial Fibrillation: Identifying Structural Remodeling by 3-D Electroanatomic Mapping Irrespective of the Rhythm. J Cardiovasc Electrophysiol. 2016 Aug;27(8):905-12.
- Yagishita A, Sparano D, Cakulev I, Gimbel JR, Phelan T, Mustafa H, De Oliveira S, Mackall J, Arruda M. Identification and electrophysiological characterization of early left atrial structural remodeling as a predictor for atrial fibrillation recurrence after pulmonary vein isolation. J Cardiovasc Electrophysiol. 2017 Jun;28(6):642-650.
- Yagishita A, Gimbel JR, DE Oliveira S, Manyam H, Sparano D, Cakulev I, Mackall J, Arruda M. Long-Term Outcome of Left Atrial Voltage-Guided Substrate Ablation During Atrial Fibrillation: A Novel Adjunctive Ablation Strategy. J Cardiovasc Electrophysiol. 2017 Feb;28(2):147-155.
- Filby SJ, Dallan LAP, Cochet A, Kobayashi A, Attizzani GF, Rashid I, Rajagopalan S, Arruda M, Shishehbor MH, Bezerra HG. Left Atrial Appendage Occlusion Using Cardiac CT Angiography and Intracardiac Echocardiography: A Prospective, Single-Center Study. J Invasive Cardiol. 2021 Oct 7:JIC20211007-1. Epub ahead of print. PMID: 34619655.


