University Hospitals Cardiogenic Shock Team, Paired with LVAD Advancements, Changes the Odds for Shock Survivors
January 25, 2021
50-50 odds of survival may grow to five to 10 more years of life
Innovations in Cardiovascular Medicine & Surgery | Winter 2021
University Hospitals Harrington Heart & Vascular Institute was the first program in Ohio to construct a coordinated, multidisciplinary Cardiogenic Shock Team for managing these most seriously ill patients, establishing the program in 2017.
 Michael Zacharias, DO
Michael Zacharias, DOThis decision, paired with advancements in left ventricular assist devices (LVADs), has had a dramatic impact on survival for patients, says Michael Zacharias, DO, Medical Director of Mechanical Circulatory Support Program and Director, Inpatient Cardiovascular Service at University Hospitals Cleveland Medical Center, and Assistant Professor at Case Western Reserve University School of Medicine. Now, he says, certain cardiogenic shock survivors who may have faced just 50-50 odds of survival may now expect to live five to 10 years, if not longer, with an LVAD.
For Dr. Zacharias, the multidisciplinary Shock Team has provided the necessary foundation for this success. ”Most of these patients would have died had it not been some of the things that we've instituted as part of the cardiogenic team here at University Hospitals,” he says. “Specific to those who go on and get an LVAD, certainly it allows them to have a completely new and improved quality of life, which they otherwise would not have been able to have. They can see their kids and grandkids grow up, go to events, do things that they otherwise couldn't have been able to do. Again, most of these people previous to this would have died in the hospital.”
How does the Shock Team at UH operate? And how are cardiogenic shock patients considered for LVAD therapy? When a patient presents with cardiogenic shock at a UH facility, the event immediately triggers a rapid response. The UH Shock Team includes physicians specializing in emergency medicine, critical care, interventional cardiology, heart failure and cardiovascular surgery, as well as expert physician assistants, nurse practitioners, nurses and respiratory therapists. On-call team members are activated through a single phone call via the UH phone transfer center and immediately convene by phone to decide the optimal front-line approach to stabilize each patient. Using a detailed algorithm that the team has developed, they evaluate the severity of shock and coordinate efforts to determine a treatment plan.
UH Harrington Heart & Vascular Institute offers 15 locations throughout Northeast Ohio that can provide front-line therapy and activate the Shock Team. Seven of these facilities also offer full heart catheterization capabilities and percutaneous mechanical heart support technologies that generates a full hemodynamic profile to inform treatment decisions. If escalation of care or a greater level of mechanical support is indicated, patients are quickly transferred within the UH system to the most suitable setting.
Next, the Shock Team evaluates whether the patient is a good candidate for an LVAD. The decision-making about potential LVAD therapy is multifactorial, Dr. Zacharias says. “The ones we consider for LVAD therapy are those who cannot come off of either IV medicines that are supporting their heart or a temporary heart pump that was placed at the time of their diagnosis of cardiogenic shock,” he says.
The team also evaluates whether kidney and liver function is intact.
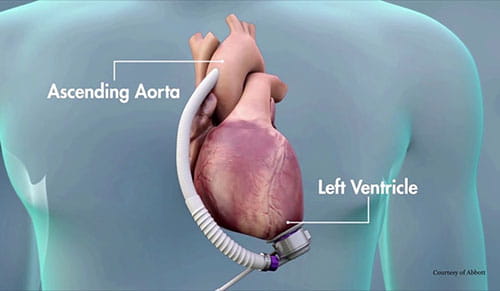 LVAD placement illustration courtesy of Abbott.
LVAD placement illustration courtesy of Abbott.
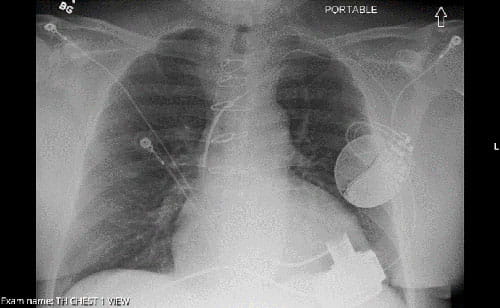 X-ray with LVAD.
X-ray with LVAD.“If both of those are in place, then we will initiate an evaluation for these patients that takes into account not only their cardiac issues, but also other comorbid medical conditions that they might have,” Dr. Zacharias says. “But equally important is their psychosocial status and their social support. Do they have people to provide support or caregivers who can support them through this, both before and then, more importantly, after they leave the hospital with this pump?”
“In the hospital it's vital that we manage their fluid levels, their blood pressure as well as their blood thinners,” he adds. “Once they leave the hospital, we’re focused on blood pressure, maintaining an appropriately anticoagulated state, making sure their blood thinners are appropriate and then monitoring for any signs of issues or complications related to the pump itself. They'll have routine follow-up in our LVAD clinic afterwards.”
In terms of results, Dr. Zacharias says the combination of excellent cardiogenic shock care and LVAD enhancements allow him to present his patients with a hopeful picture.
“I tell people, assuming everything goes well and we can maintain their blood pressure and their blood thinner levels, I would expect five to 10 years survival, if not longer,” he says. “Even with the old pump, we've had patients in our particular program here at UH who have lived almost up to 10 years with their pump.”
He credits the team approach at UH for making this possible. “From the time that we hear about the patient, whether they're at an outside hospital or one of our community hospitals, or even at our flagship UH Cleveland Medical Center, it's a multidisciplinary discussion about what's the best way to approach these patients,” Dr. Zacharias says. “That's allowed us to use new technology and take into account a variety of factors from different specialists on how best to manage these patients. So we've actually given these patients a chance to be able to go to a durable LVAD and ultimately go on and leave the hospital. Before, it'd be a flip of a coin, whether they’d be alive or dead. And now we're giving an additional potential five to 10 years, which is pretty impressive.”


