Expanding Diaphragm Respiratory Pacing
March 04, 2020
UH is at the forefront of innovations to boost quality of life
Innovations in Pulmonology & Sleep Medicine | Winter 2020
 Raymond Onders, MD
Raymond Onders, MDFor patients with spinal cord injuries or sleep apnea, diaphragm respiratory pacing (diaphragm pacing) can provide nonmechanical ventilation support and improved quality of life.
“University Hospitals Cleveland Medical Center developed diaphragm pacing more than 20 years ago and is the world’s premier center at helping patients breathe when they can’t move their diaphragm,” says Raymond Onders, MD, Division Chief, General and Gastrointestinal Surgery, and Remen Chair in Surgical Innovation, UH Cleveland Medical Center; Professor of Surgery, Case Western Reserve University School of Medicine.
University Hospitals initially began using diaphragm pacing for patients with high spinal cord injuries (above C2, C3) who couldn’t breathe but who had an intact phrenic nerve.
“We were able to replace the tracheostomy and mechanical ventilation with diaphragm pacing, which allows more natural breathing with negative pressure ventilation,” Dr. Onders says.
Since then, the uses of diaphragm pacing have expanded and now include patients with central sleep apnea, patients with diseases such as amyotrophic lateral sclerosis or spinal muscular atrophy, and patients who have failure to wean from mechanical ventilation following lung, cardiac, or liver transplant.
“Diaphragm pacing also helps patients with shortness of breath from an elevated diaphragm, where the phrenic nerve is injured from cardiac surgery, or idiopathic cases, ones where patients develop shortness of breath all of a sudden,” says Dr. Onders.
Today, about 2,000 patients worldwide have a diaphragm pacing device, and UH alone has performed the procedure in more than 700 patients. Dr. Onders and his colleagues have widely presented and published their results.
DIAPHRAGM PACING TECHNOLOGY AN OUTPATIENT PROCEDURE
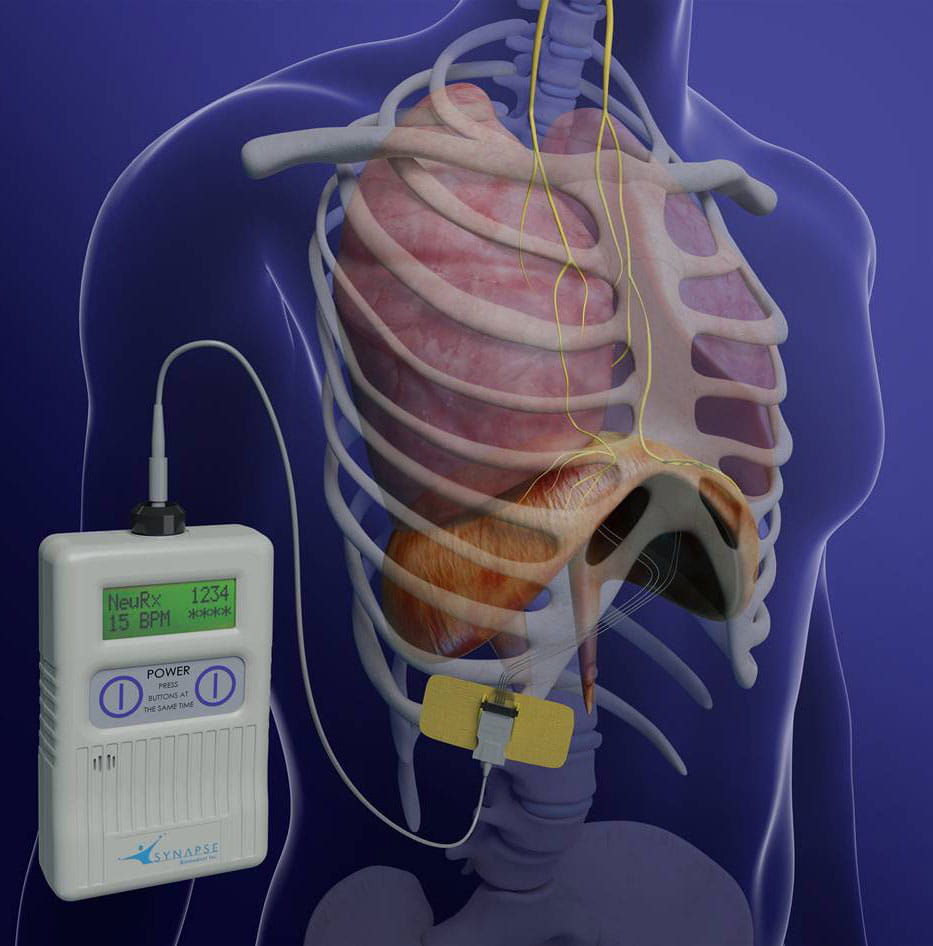
Implanting the diaphragm pacing technology is an outpatient laparoscopic procedure. Electrodes surgically implanted on the diaphragm are attached to a receiver and an external box with an antenna on the skin’s surface. The pacing and other settings are optimized for each patient.
Immediately after surgery, the patient’s diaphragm can begin the reconditioning through electrical stimulation to increase muscle strength. The length of time required to condition the diaphragm depends on the time from injury and the amount of daily training.
ADVANTAGES OF DIAPHRAGM PACING
Among the benefits of diaphragm pacing are:
Lower mortality and length of hospital stay. Diaphragm pacing lowers the risks (and associated high costs) of tracheostomy complications, such as ventilator-associated pneumonia (the greatest cause of decreased life expectancy) and prolonged mechanical weaning. It also lessens patients’ risks for tracheal injury from the ventilation tube.
Decrease in ventilator days. Dr. Onders says patients on diaphragm pacing have fewer days on mechanical ventilation and statistically significant increases in spontaneous tidal volume compared with patients with no diaphragm pacing. Furthermore, the sooner patients begin diaphragm pacing, the sooner they can be removed from a ventilator and begin rehabilitation for spinal cord injuries.
Patient preference. Free from the burden of mechanical ventilation, patients have greater independence to move about, perform activities of daily living and, in some cases, even return to work. Without an endotracheal tube, patients can also speak — a huge advantage.
Flexibility. Diaphragm pacing can be used for both short- and long-term ventilation assistance.
Dr. Onders has patients with spinal cord injuries who have used diaphragm pacing continuously for 20 years to maintain a ventilator-free life.
"Newer models allow us to use temporary diaphragm pacing just until a patient recovers from diaphragm dysfunction or nerve injury,” he says. “Then we simply remove the electrodes percutaneously.”
ENCOURAGING RESULTS
Diaphragm pacing is safe and durable, says Dr. Onders. For example, in a multicenter review of diaphragm pacing in patients with spinal cord injuries published in the Journal of Trauma Acute Care Surgery, 82 percent of patients with implants were completely weaned from a ventilator, and 36 percent completely recovered diaphragm respiration and had their diaphragm pacing wires removed.1
UH continues to be at the forefront of diaphragm pacing innovations.
“Currently, we’re studying new [Food and Drug Administration]-approved diaphragm pacing technology to shorten ventilation time after a major cardiac procedure,” says Dr. Onders. “We place electrodes at the time of open-heart surgery in high-risk cardiac patients, those whom we expect to need prolonged mechanical ventilation. We can maintain their diaphragm strength through electrical stimulation during recovery, so their diaphragm does not atrophy.”
To schedule an appointment for diaphragm pacing or to contact Dr. Onders, call 216-553-1649.
1Posluszny, Joseph A. Jr.; Onders, Raymond; Kerwin, Andrew J.; Weinstein, Michael S.; Stein, Deborah M.; Knight, Jennifer; Lottenberg, Lawrence; Cheatham, Michael L.; Khansarinia, Saeid; Dayal, Saraswati; Byers, Patricia M.; Diebel, Lawrence. Multicenter review of diaphragm pacing in spinal cord injury: Successful not only in weaning from ventilators but also in bridging to independent respiration. Journal of Trauma and Acute Care Surgery. 76(2):303-310, February 2014.


