UH Vascular Surgeon Frees Young Patient from Rare and Dangerous Congenital Anomaly
November 07, 2023
Innovations in Cardiovascular Medicine & Surgery | Fall 2023
The ability to manage rare, complex cases is par for the course at University Hospitals (UH) Harrington Heart & Vascular Institute. A recent patient successfully treated by Karem Harth, MD, vascular surgeon and Director of the Center for Comprehensive Venous Care, and her team is just one example. It’s estimated that the condition facing the patient affects less than 0.6 percent of the population.
The 28-year-old woman arrived for care at UH Cleveland Medical Center after two outside hospitals could not address her unusual condition leading to her significant leg pain and swelling. At one outside institution, the patient had received a left lower extremity ultrasound scan for deep vein thrombosis (DVT), which was positive along the entire left leg, and a CT scan performed, which additionally confirmed a blood clot all the way up to the level of her liver where her IVC then became atretic.
“The patient presented to us at UH with left leg phlegmasia due to IVC and bilateral iliofemoral DVT which was confirmed on duplex and CT scan,” Dr. Harth says.
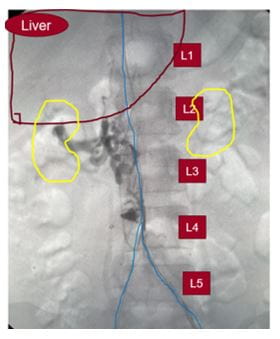 Congenital anomaly before intervention
Congenital anomaly before intervention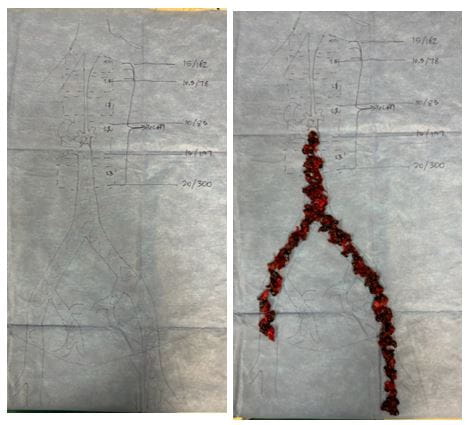 During thrombectomy procedure.
During thrombectomy procedure.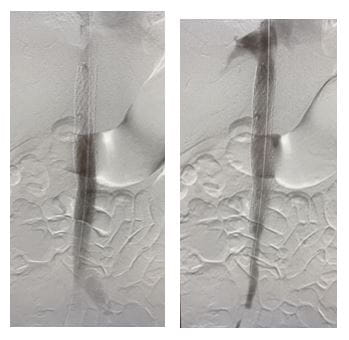 After stenting.
After stenting.Her overall clinical history, presentation and imaging was consistent with the patient having a congenital occlusion of the retro-hepatic inferior vena cava, the portion of the major vessel lying behind the liver.
“Those of us who see DVT, when we think of phlegmasia, we think of ilac or pelvic vein DVT,” Dr. Harth says. “This was certainly not one of those routine cases.”
“There are different anatomic variants of congenital IVC anomalies, primarily from an abnormal regression or persistence of the embryologic veins,” she adds. “Although most anomalies are asymptomatic, they can cause lower extremity venous insufficiency, deep vein thrombosis, pelvic congestion syndrome and can affect the planning of vascular procedures, so they’re really important to identify. With our case, this particular anatomy has a prevalence of less than 0.6 percent.”
To address the problem, Dr. Harth performed a staged complete IVC and bilateral iliofemoral thrombectomy and recanalization. In addition, she reconstructed the patient’s congenitally occluded retro-hepatic IVC with IVC stenting.
“Repeat mechanical thrombectomy with a larger device of the residual thrombus allowed us to remove more of the chronic, sub-acute thrombus that we couldn’t remove with suction thrombectomy,” Dr. Harth says. “We then proceeded to dilate up her retro-hepatic IVC which originally started off as an occluded vessel, to a 20 mm diameter with intravascular ultrasound and venographic guidance and ultimately deployed a 20 mm stent.”
“The rarity of this case and the ability to perform a completely minimally invasive reconstruction is exemplified by the fact that such cases are at best case reports in our literature,” she adds. "Most patients will only be treated medically and develop post-thrombotic syndrome, which is a disabling condition manifested by painful swelling and walking and in severe cases can lead to leg ulceration.”
Since the successful procedure, things have been looking up for Dr. Harth’s patient.
“I saw last week in clinic, and she’s doing great,” she says. “At her two week post-visit, she was tolerating her blood thinners and had no leg edema and no symptoms. Follow-up scans show a nice, beautiful open stent. I’m looking forward to seeing her back in four to six weeks. I’m also very excited about our ability to take care of complex patients like this and the support we receive from UH Harrington Heart & Vascular Institute.”
“This is the kind of case we would not be doing here at UH, with this level of complex, venous work, before Dr. Harth decided to commit to this path, and with the commitment to create the Center for Comprehensive Venous Care,” says Mehdi Shishehbor, DO, MPH, PhD, President, UH Harrington Heart & Vascular Institute and Angela and James Hambrick Chair in Innovation. “Look where we are. It’s a beautiful example of how physicians, supported by our administrative team, continue to fight, to learn, to grow.”
Congratulations to Dr. Harth on a successful and rewarding case.
Contributing Expert:
Karem Harth, MD
Director of the Center for Comprehensive Venous Care
UH Harrington Heart & Vascular Institute
Associate Professor of Surgery
Case Western Reserve University School of Medicine
Tags: Vascular Disease


