Multi-Disciplinary Care for Patients with Primary and Metastatic Tumors of the Brain & Spine
May 16, 2018
University Hospital’s Neurological Institute works closely with UH Seidman Cancer Center to offer cutting-edge treatments for primary and metastatic cancers of the brain and spine and for non-metastatic neurological complications in cancer patients. The multi-disciplinary team is comprised of neurosurgeons, neuro-oncologists, medical oncologists, and radiation oncologists.
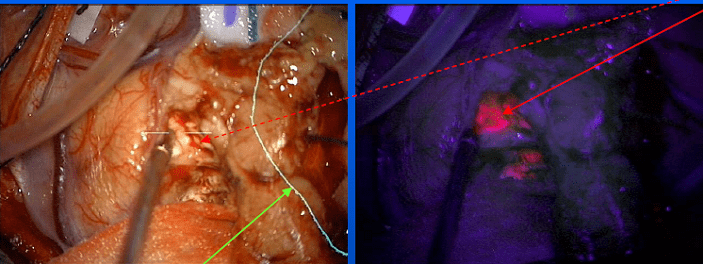
Andrew Sloan, MD, Director, Brain Tumor and Neuro-Oncology Center (BTNOC), Peter D. Cristal Chair of Neurosurgical Oncology, and Vice Chairman of Neurological Surgery, noted that new and innovative approaches to surgery often help improve the extent of resection in brain tumors. 5-Aminolevulinic acid (5-ALA) is given prior to surgery and makes the tumor fluoresce pink for more precise identification of its borders. A newer approach using cell-surface protein tyrosine phosphatase mu (Ptpu), funded by a grants to Dr. Sloan & collaborators by the Coulter Fund and the National Institute of Health (NIH), may be even more tumor specific.
“This is important because where the tumor ends and normal brain begins is not always obvious to the surgeon. Importantly, of the five prognostic indicators that determine survival for brain cancer, extent of resection is the only one that physicians can influence,” Dr. Sloan said. Leaving even a small amount of tumor behind greatly decreases a patient’s survival.
In case there is any doubt, a high-powered 3T intra-operative MRI? one of the first in Ohio? also allows the surgeon to check for residual tumor before completing the surgery.
Another cutting-edge technique pioneered at UH is Laser Interstitial Thermotherapy (LITT), a minimally invasive way to treat brain tumors using lasers guided by MRI, rather than the surgeon’s eyes. UH surgeons also are also now injecting oncolytic viruses into the tumor bed after resection to cause an immune response that kills any infiltrating tumor cells left behind after surgery.
UH is a member of the elite 10 Brain Tumor Centers of Excellence known as the Adult Brain Tumor Consortium (ABTC), and UH investigators have led trials in the group as well as in the NRG Consortium. These include the recently completed trial of immunotherapy drugs known as checkpoint inhibitors – used alone or together – for the treatment of glioblastomas (GBM). In addition, Dr. Sloan recently received funding to combine LITT with immunotherapy for patients with GBM. Lisa R. Rogers, DO, Medical Director of the Neuro-Oncology Program, leads many of the chemotherapy trials for primary tumors including a trial of the ketogenic diet.
Adjuvant radiation at UH includes proton beam radiotherapy, which may be associated with less toxicity than conventional radiation, as well as stereotactic radiosurgery using gamma-knife or Cyber-knife delivered in collaborations with our radiation oncologists.
COMPLICATIONS OF SYSTEMIC CANCER
The multidisciplinary team is also involved in the evaluation and treatment of brain metastases, a common complication of cancer that effects an estimated 500,000 cancer patients in the United States annually.
Fortunately, there are emerging technologies and medical treatments for such patients. A limited number of metastases can be treated by surgical resection and/or radiosurgery. Dr. Rogers collaborates with staff from radiation oncology and medical oncology at UH to enlist patients in clinical trials, studying the potential benefit of alternating electrical fields in combination with radiosurgery and a radiosensitizer with whole brain radiation. There is an expanding role for drugs targeting mutations within the cancer and also check point inhibitors available in standard practice and in clinical trial. UH Seidman Cancer Center has a very large Phase I clinical trial portfolio for selected patients.
Non-metastatic neurological complications are a common cause of diminished quality of life in cancer patients, including impaired cognition following whole brain radiation for brain metastasis or following chemotherapy for systemic cancer (“chemo brain”). UH provides a weekly neuro-oncology clinic to evaluate cancer patients with cognitive complaints. Same day neuropsychology testing is performed to identify the cause and members of the Supportive Oncology team can assess for potentially reversible factors.
Increasing MRI enhancement following radiosurgery for brain metastasis can indicate recurrent tumor or radiation necrosis. Radiation necrosis can produce mass effect in the brain and lead to reduced quality of life and survival. Dr. Rogers and members of radiology at UH and Biomedical Engineering at Case Western Reserve University are collaborating on noninvasive methods to identify radiation necrosis; a combination of MRI studies, including PET, perfusion and textural analysis, is highly accurate. Dr. Sloan is developing a “liquid biopsy”, using blood to differentiate recurrent tumor from changes induced by treatment. UH offers anti-angiogenic therapy and hyperbaric oxygen to treat radiation necrosis.
Dr. Rogers collaborates closely with the UH Seidman Cancer Center’s Integrative and Supportive Oncology Program, to provide a multidisciplinary approach to peripheral neuropathy caused by chemotherapy or by immunotherapy. In addition to medical therapy to reduce symptoms, a formal trial of acupuncture in selected patients is planned for the summer of 2018.
NEWEST TEAM MEMBER

Tiffany R. Hodges, MD, a neurosurgeon who completed her Neurosurgical Residency at Duke University and Neurosurgical Oncology Fellowship at MD Anderson Cancer Center, joined the team in August 2017. She brings with her expertise and experience in primary and metastatic brain tumor epidemiology research, clinical outcomes and novel approaches to spinal metastasis. She has published in several national journals on her previous glioblastoma research, and enjoys teaching the next generation of neurosurgeons. “Dr. Hodges is a great addition to the team, and greatly improves access to care,” noted Dr. Sloan. The addition of Dr. Hodges highlights University Hospitals’ commitment to providing the best possible care to patients with tumors of the brain and spine.
Tiffany R. Hodges, MD
University Hospitals, Cleveland, Ohio
Neurological Surgery - Oncology
Clinical Assistant Professor, Neurosurgery
Case Western Reserve University School of Medicine


