Improving gynecological laparoscopy operative reporting
February 09, 2019
UH study explores the impact of standardization on communication, patient care in gynecological laparoscopy cases
Innovations in Obstetrics & Gynecology - Winter 2019
Communication between clinicians across all specialties is core to quality care. In recognition of that, a team of University Hospitals Cleveland Medical Center physicians and researchers set out to examine if the standardization of laparoscopic operative reporting could improve gynecological surgeons’ communication.
 Kristine Zanotti, MD
Kristine Zanotti, MDUNCOVERING VARIATION
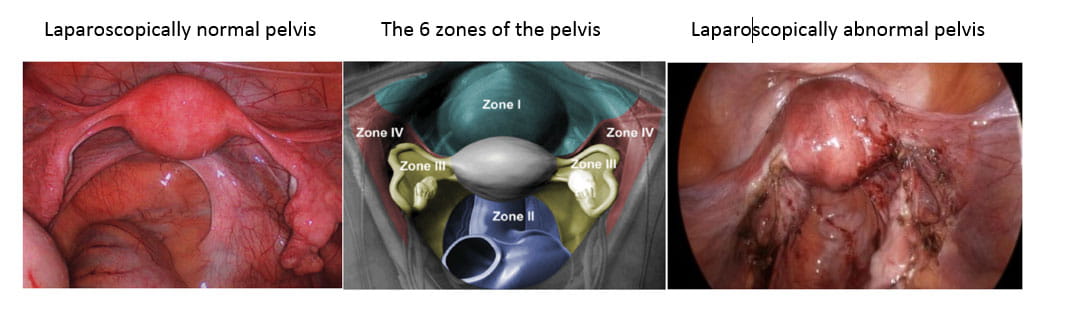
Standard operative reporting, or “the operative note,” typically includes many details, including a rationale for the surgery, a description of the surgical findings and a description of the surgical steps taken. Operative reporting for simple, straightforward procedures can easily fit into a template, but this process becomes much more variable for complex surgeries. UH researchers found the most variation within the operative note for gynecologic laparoscopy cases occurs in the “surgical findings” section.
“The visual findings identified during a laparoscopic procedure have the potential to provide a significant diagnostic function,” says Kristine Zanotti, MD, Director of the Gynecologic Oncology Fellowship in the Department of Obstetrics and Gynecology at UH Cleveland Medical Center. “As such, the effective communication of these findings should be taken as seriously as the communication of visual findings on a radiology study or on a diagnostic procedure such as a colonoscopy. If surgical findings are not communicated well to others also caring for the patient, then this is a significant opportunity lost.”
Upon recognizing that variability, Dr. Zanotti and her team pioneered a study to explore opportunities for standardization. “We wanted to see if we could improve the quality and completeness of this reporting by providing a template for standardization of reporting of visual findings at gynecologic laparoscopy,” explains Dr. Zanotti, study author.
The study, conducted at UH Cleveland Medical Center, included 15 surgeons across gynecological oncology, reproductive endocrinology, and general obstetrics and gynecology. Eighty surgical cases were included in the final analysis.
A NEW SYSTEM FOR COMMUNICATION
At the beginning of the study, UH researchers held a brief educational session for the participating surgeons. During the session, Dr. Zanotti and her team described a process for routinely describing both positive and negative surgical findings divided across six anatomically distinct zones of the pelvis. Over the course of the next year, the participating surgeons were asked to use this system for their reporting.
Afterward, the UH team studied the surgeons’ operative reporting and scored them for accuracy and completeness.
“We found that providing a simple template that would allow structure to the reporting of surgical findings yields much more consistent results and better content across the board,” Dr. Zanotti says.
Consistency combined with higher quality of operative reporting translates into improved communication and patient care without requiring an intensive time commitment from surgeons.
INCORPORATING RESULTS INTO RESIDENT TRAINING
The results of the study reveal that standardization does have the power to improve operative reporting, and by extension communication, in gynecological laparoscopy cases. The study results also reveal a useful application for this type of standardization.
“One of the findings suggests that it would be more impactful to include this approach in the surgical training of residents,” Dr. Zanotti says.
The next steps will be to incorporate the type of educational session used in study into the training for surgical residents. From there, residents can carry their training in improved operative reporting with them in their daily practice.
“UH always emphasizes communication as a path to quality care,” Dr. Zanotti says. “I think that this quality improvement aligns very well with this mission.”
INNOVATION IN SURPRISING PLACES
Innovation often comes with the expectation of exciting discoveries and changes driven by the latest in technology. While innovation certainly has its place there, the small changes that come from actionable research can also have a big impact.
“This study highlights the fact that you can find quality innovations anywhere,” Dr. Zanotti notes. “Innovation does not necessarily require tremendous technology application. Instead, real innovation can be found with a fresh look at routine practice.”
Contact Dr. Zanotti at ObGynInnovations@UHhospitals.org.


