Endoscopic Submucosal Dissection for Small, Early-stage Tumors
February 18, 2019
University Hospitals Digestive Health Institute is among few using this minimally invasive approach to treat gastric cancer
Innovations in Digestive Health – Winter 2019
 John Ammori, MD
John Ammori, MD John Dumot, DO
John Dumot, DOAlthough stomach cancer rates in the United States have declined since the early 20th century, it remains a concern, especially for black, Asian and Native American populations. Surgery is the standard treatment for stages 0 through III cancer; however, surgical oncologists and gastroenterologists are adopting minimally invasive approaches with greater frequency.
UH Digestive Health Institute gastroenterologists and UH Seidman Cancer Center surgeons partner to offer one the few centers with physicians experienced in minimally invasive approaches to stomach cancer. John Dumot, DO, FASGE, Director of UH Digestive Health Institute and Professor of Medicine, Case Western Reserve University School of Medicine, has extensive experience in endoscopic submucosal dissection (ESD). John Ammori, MD, a member of the Gastrointestinal Surgery and Surgical Oncology team at UH Cleveland Medical Center and Associate Professor of Surgery for the School of Medicine, performs laparoscopic surgery for gastric cancer.Endoscopic Approach for Early Gastric Cancer
Many physicians in Asia use endoscopic mucosal resection to treat dysplasia and early gastric cancers because of its low risk of lymph node metastasis.1 ESD, however, is a relatively new gastric cancer treatment in the United States. University Hospitals recommends ESD for small, early-stage tumors that are at low risk for lymph node metastases.
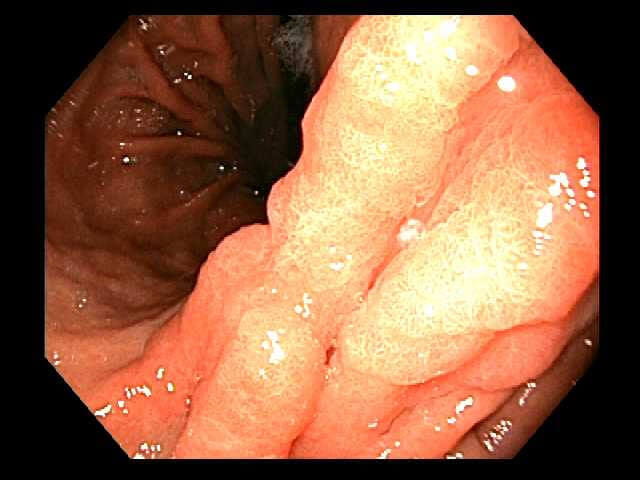 An early gastric cancer is noted on the lesser curve of the stomach.
An early gastric cancer is noted on the lesser curve of the stomach. Endoscopic ultrasound confirmed the lesion was confined to the gastric wall without lymphadenopathy.
Endoscopic ultrasound confirmed the lesion was confined to the gastric wall without lymphadenopathy.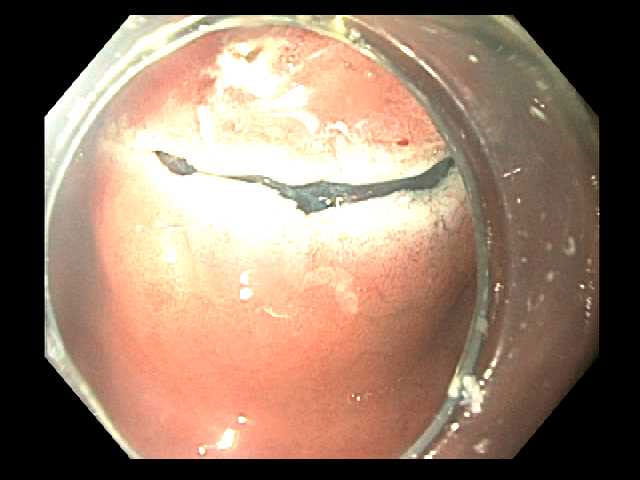 The initial incision is made after marking the margins of the lesion and injecting fluid into the submucosal layer.
The initial incision is made after marking the margins of the lesion and injecting fluid into the submucosal layer.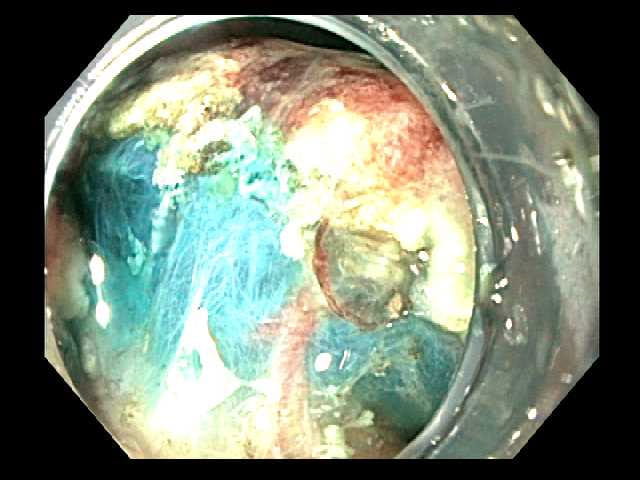 Submucosal dissection is aided by injection of fluid with methylene blue.
Submucosal dissection is aided by injection of fluid with methylene blue. Submucosal dissection causes the lesion to retract away from the gastric wall exposing the deeper muscularis propria layer.
Submucosal dissection causes the lesion to retract away from the gastric wall exposing the deeper muscularis propria layer. The distal margin of the resection site is adjacent to the pylorus.
The distal margin of the resection site is adjacent to the pylorus.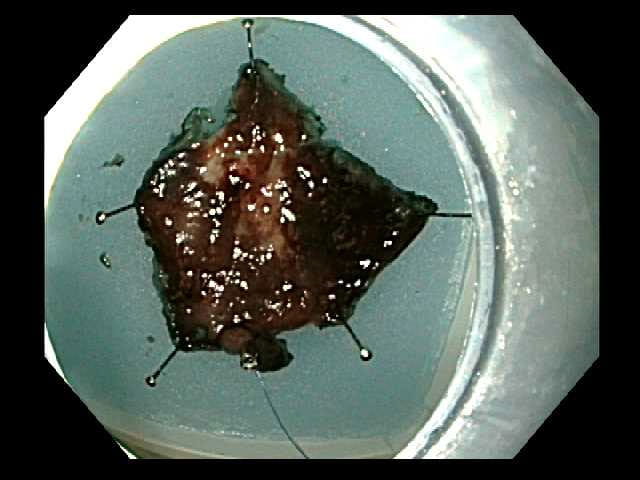 The specimen is prepared by pinning to a paraffin tray for assessment of peripheral and deep margins.
The specimen is prepared by pinning to a paraffin tray for assessment of peripheral and deep margins. 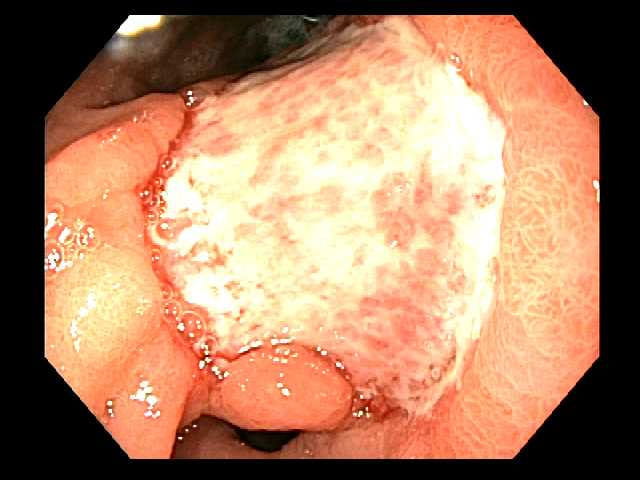 Follow up endoscopy after submucosal dissection site at 3 weeks.
Follow up endoscopy after submucosal dissection site at 3 weeks.During an ESD procedure, a gastroenterologist uses an endoscope and fluid injected into the submucosal layer to lift the tumor from the muscular layer in the gastric wall. This minimizes damage to surrounding tissue. The physician then uses an electrosurgical knife to remove the tumor. Most patients go home the same or next day.
Dr. Dumot learned ESD techniques eight years ago in Japan, a country that pioneered endoscopic gastric cancer treatment. Because Japan has one of the highest stomach cancer rates in the world, the country has adopted widespread screening programs and developed novel treatments.
The advantages of ESD over open surgery are similar to many non-invasive approaches: shorter operating time, shorter hospital stay, shorter recovery time and fewer complications.2 “We try to offer the latest care in a somewhat conservative fashion,” Dr. Dumot says. “Patients have to be well-selected for minimally invasive surgery and understand the advantages and disadvantages.”
The Laparoscopic Approach for Advanced Cancers
Studies have demonstrated the safety of laparoscopic gastrectomy for advanced cancer treatment. Instead of one large cut, laparoscopy allows surgeons to remove the stomach through several small incisions while guided by a laparoscope.
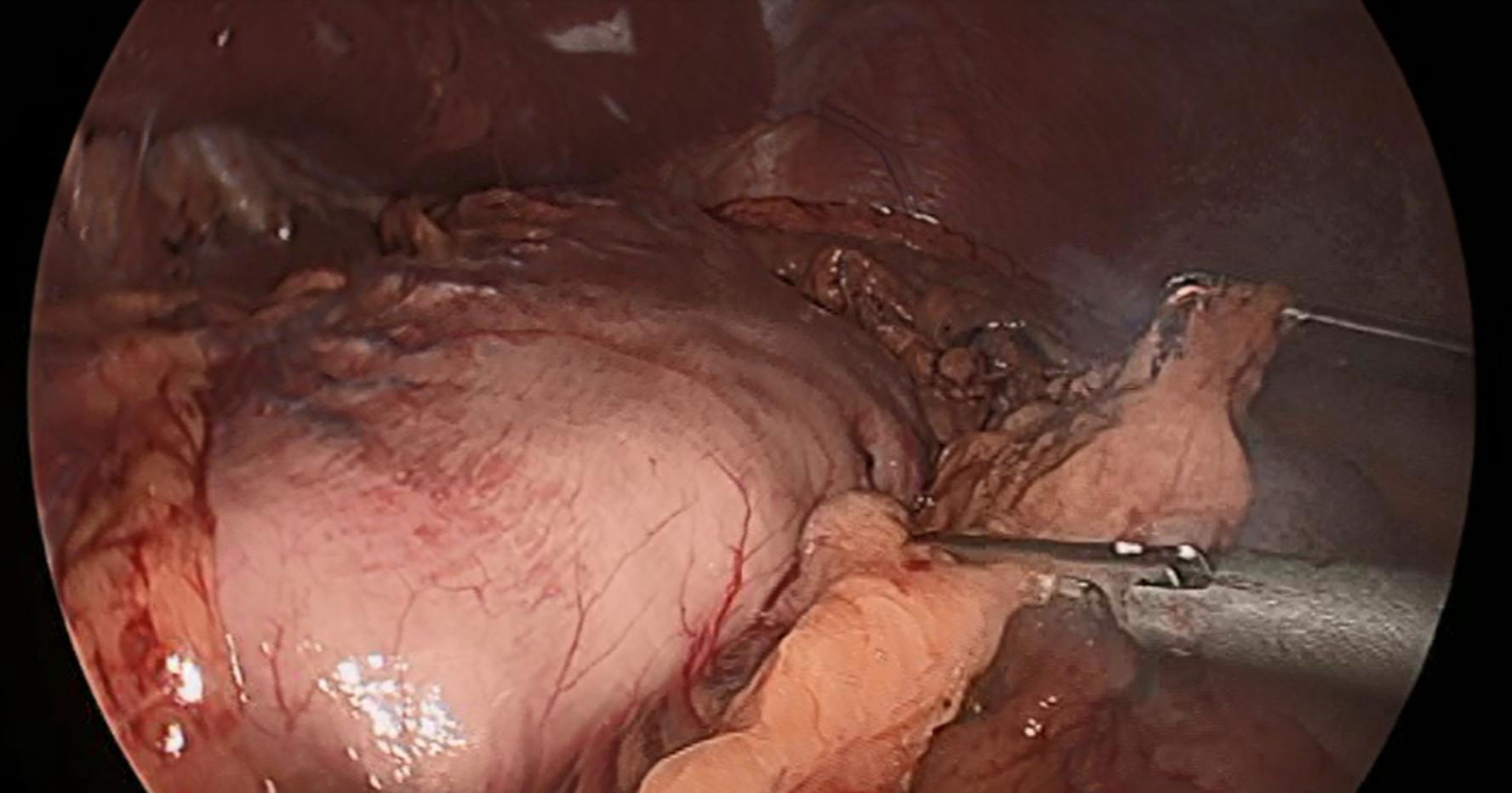 Laparoscopic view of the stomach
Laparoscopic view of the stomach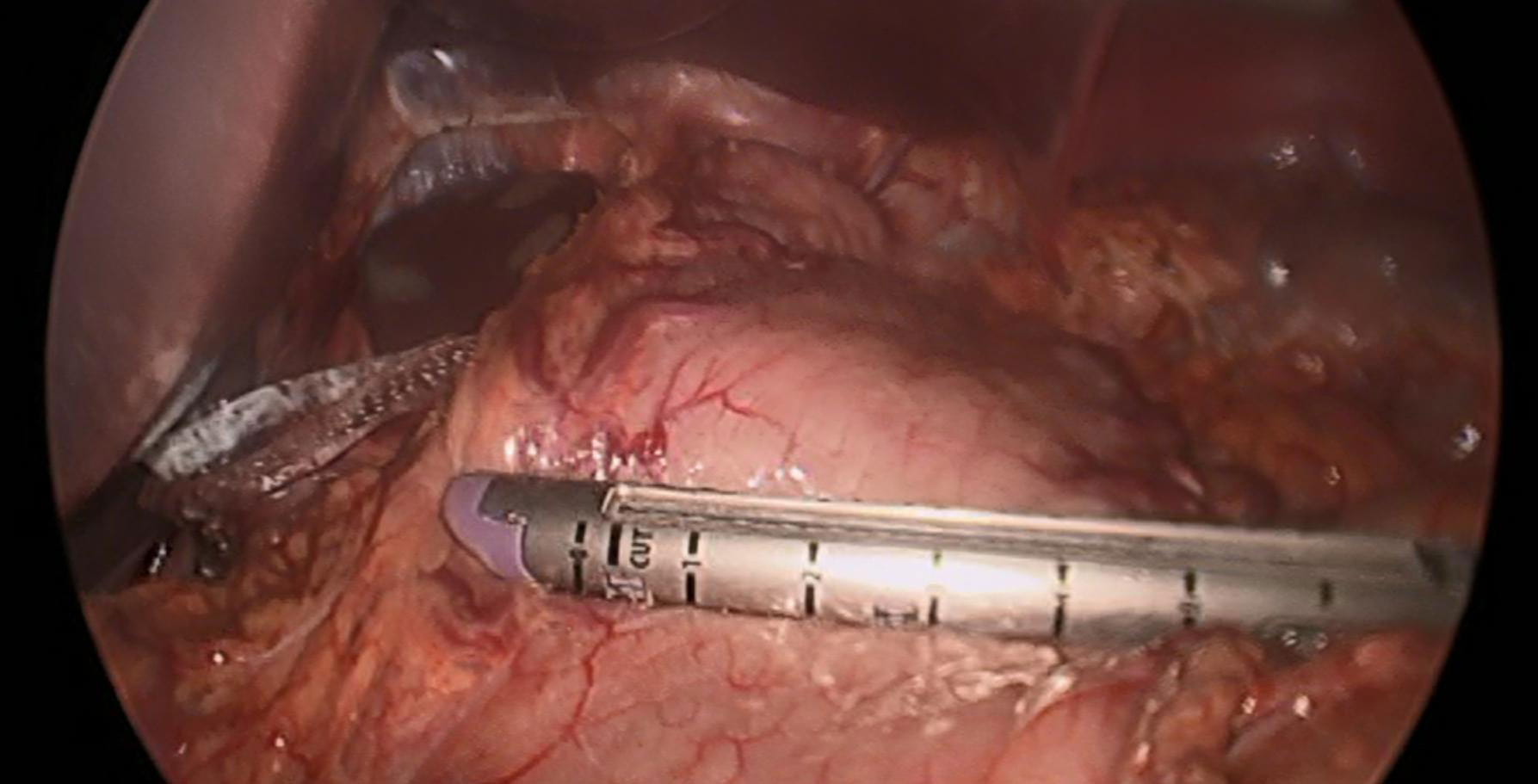 Laparoscopic view of a surgical stapler on the stomach
Laparoscopic view of a surgical stapler on the stomach Laparoscopic view of the completed gastrojejunal anastomosis after distal gastrectomy
Laparoscopic view of the completed gastrojejunal anastomosis after distal gastrectomy“Over the past 10 to 15 years, more types of operations are being done laparoscopically,” Dr. Ammori says. “More surgeons have gained experience in the technique and it’s become a more accepted way of treating cancer.”
Studies have reported the following advantages of laparoscopic gastrectomy over open surgery:
- Less blood loss
- Quicker time to walking and first oral intake
- Reduced pain
- Shorter hospital stays
- Lower overall postoperative morbidity
“There is no difference in the number of retrieved lymph nodes, mortality, recurrence, long-term overall survival and disease-free survival between laparoscopic and open gastrectomy,” Dr. Ammori adds.
A Team Effort
University Hospitals takes a multidisciplinary team approach to treat gastric cancer. As with other cancers, the gastric cancer team has a multidisciplinary tumor board. The board includes medical, surgical and radiation oncology, gastroenterology, radiology and pathology.
The tumor board meets once a week to discuss all patients. “All our patients get presented,” Dr. Ammori says. “We can review a patient’s history, pathology and scans, put our minds together and decide on the best treatment plan for that patient.”
UH’s collaborative approach also comes into play outside of the conference room. In one case, Dr. Dumot performed ESD on a man in his mid-50s with early gastric cancer. During the procedure, he found a 1.5 cm invasive adenocarcinoma as well as other areas of invasive cancer. The margins of ESD were also positive.
Based on these findings, Dr. Dumot recommended laparoscopic distal gastrectomy and lymphadenectomy, which Dr. Ammori performed. Results showed clear margins and no metastatic disease to the lymph nodes.
“This is a good example of using ESD when the pathology and tumor characteristics are appropriate — and following that with another minimally invasive approach when the ESD pathology showed more extensive disease,” Dr. Ammori says.
This patient and others benefit from the latest innovations in stomach cancer treatment. “With minimally invasive gastric cancer surgery, it’s a matter of not only having experienced surgeons, but also surgeons who understand gastric cancer,” Dr. Ammori says. “We’re offering the most advanced, least invasive types of treatment that offer the best outcomes.”
To refer a patient for gastric cancer screening, call 216-844-ENDO(3630).


