Demystifying Enlarged Vestibular Aqueduct Syndrome
September 15, 2016

New national EVA patient registry will clarify prognosis, identify risk factors for EVA-related hearing loss
Innovations in Pediatrics - Summer 2016 - View Full PDF
 Todd Otteson, MD, PhD
Todd Otteson, MD, PhDIt’s a clinical conundrum: An enlarged vestibular aqueduct (EVA) is the most common inner ear malformation linked to sensorineural hearing loss in children. Yet pediatric otolaryngologists know relatively little about how and why EVA syndrome progresses to hearing loss – and which interventions might stop the process. Some patients develop profound hearing loss, while others do not – a difference seemingly unrelated to the size of the EVA.
“Much of what is known about EVA syndrome comes from small studies of fewer than 100 people,” says Todd Otteson, MD, MPH, Division Chief, Pediatric Otolaryngology, University Hospitals Rainbow Babies & Children’s Hospital; Associate Professor, Otolaryngology and Associate Professor of Pediatrics, Case Western Reserve University School of Medicine. “Because of this, there’s a lack of reliable information we can give patients and families about how much hearing loss will occur and how it will – or will not – progress.”
The dearth of patient data may be a result, at least in part, of past limitations in imaging EVA. Until recently, Dr. Otteson says, imaging technology was inadequate to accurately characterize an EVA.
“Our data on EVA is only as good as the accuracy of our imaging,” he says. “Vestibular anatomy has a size on the order of millimeters. But advances in technology have allowed us to hone in on a clear characterization. The increasing resolution of CT scans in recent years has increased diagnosis and recognition of EVA syndrome.”
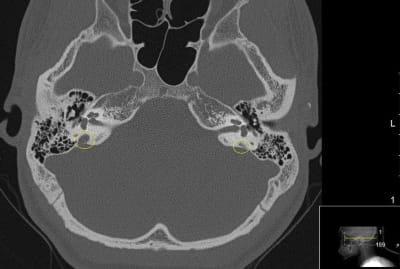 This CT scan shows a patient with an enlarged vestibular aqueduct (EVA) within the right inner ear (left on this image). Note the difference in size of the enlarged vestibular aqueduct circled in yellow on the left of the image, as compared with the normal vestibular aqueduct on the right.
This CT scan shows a patient with an enlarged vestibular aqueduct (EVA) within the right inner ear (left on this image). Note the difference in size of the enlarged vestibular aqueduct circled in yellow on the left of the image, as compared with the normal vestibular aqueduct on the right.
At UH Rainbow, Dr. Otteson and otolaryngology colleagues from the UH Ear, Nose & Throat Institute are working to shed light on this problem with a new, national EVA patient registry. Parents of children diagnosed with EVA are invited to complete a detailed online questionnaire, featuring several open-ended questions that encourage them to describe their child’s experiences.
Items cover when and how the child was diagnosed with hearing loss, if and how the loss has progressed, and whether the child has received any treatment for EVA-related hearing loss, such as steroids. Also included are questions on any family history of hearing loss or EVA syndrome and the child’s history of airplane flights, head trauma, vertigo symptoms and use of assistive services or devices, such as speech therapy, hearing aids or cochlear implants. Parents can also upload hearing test results and CT and MRI scans directly to the site. If they choose, they can also download, print, sign and mail or upload a form authorizing their treating otolaryngologist to release the child’s medical records and Personal Health Information (PHI) to the UH Rainbow EVA registry.
“This registry will help address fundamental questions regarding EVA, such as radiological definition, the safety of pressure changes that accompany airplanes or swimming, the expected progression of hearing loss over time, and the correlation of hearing loss to vestibular width,” Dr. Otteson says. “Such questions remain controversial, and this large, centralized repository of patient information will advance our current understanding.”
Dr. Otteson and his otolaryngology colleagues at the UH Ear, Nose & Throat Institute plan to make the EVA patient registry data available to otolaryngology researchers at other institutions who present study proposals approved by their Institutional Review Boards (IRBs).
“This is one of those areas where collaboration is vital,” he says. “By collecting this data from patients across the U.S., we hope to identify those events and modifiable risk factors that can be monitored, with the goal of slowing or stopping the progression of EVA-related hearing loss.”
To learn more about the UH Rainbow EVA Patient Registry, go to Rainbow.org/EVAResearch. Or email Todd.Otteson@UHhospitals.org or EVA Project Manager Mustafa.Ascha@UHhospitals.org.
Tags:


