Endoscopic Submucosal Dissection
January 04, 2016
Removing early cancers of the esophagus, stomach and colon
UH Digestive Health Institute – January 2016
 John Dumot, DO, FASGE
John Dumot, DO, FASGE Amitabh Chak, MD, FASGE
Amitabh Chak, MD, FASGE
The goal of ESD is to remove lesions or neoplastic growths in one piece (also known as en bloc). These are growths that have clear lateral and deep margins. This can be achieved when the neoplasm is of favorable histology (well or moderately differentiated) and involves only the most superficial layers of the gastrointestinal tract. Deeper invasion or poorly differentiated neoplasms require more traditional surgical approaches, or a combination of radiation and chemotherapy.
 Esophagus with early squamous cell cancer, shown with high-definition white light
Esophagus with early squamous cell cancer, shown with high-definition white light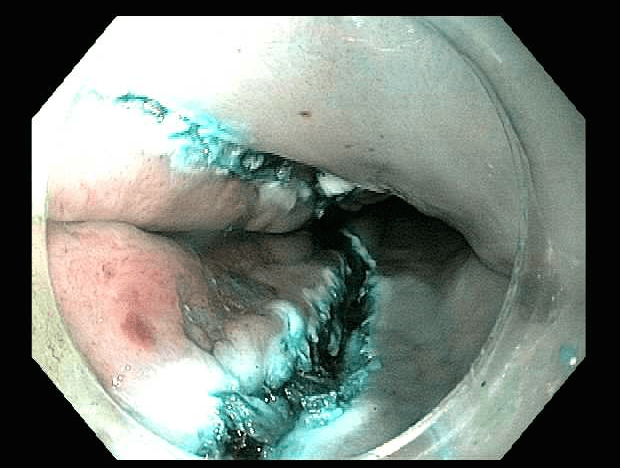 Initial circumferential incision
Initial circumferential incision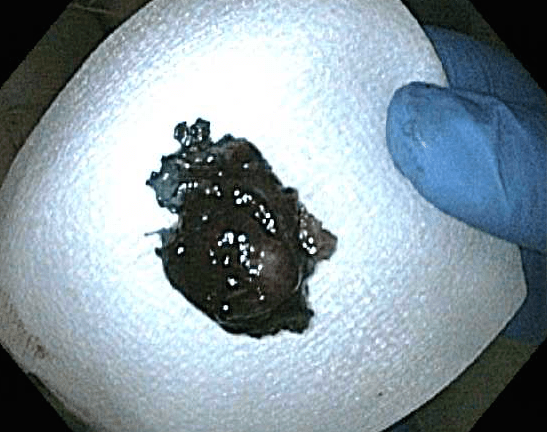 Resectioned specimen
Resectioned specimen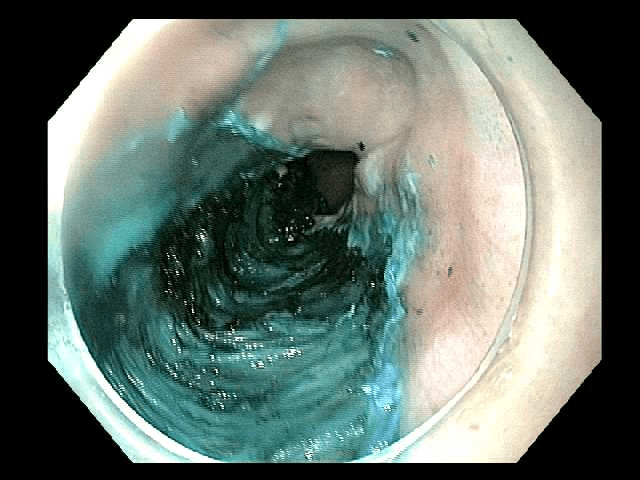 Fresh ESD site with squamous cell cancer removed
Fresh ESD site with squamous cell cancer removed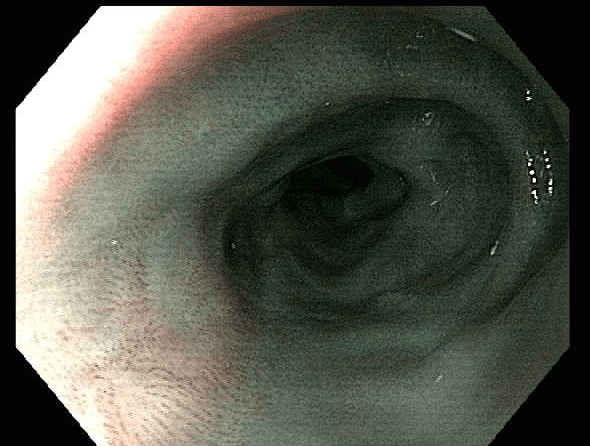 Three-month follow up exam – ESD scar and healing
Three-month follow up exam – ESD scar and healing
After the procedure, the patient was hospitalized for observation due to symptoms of chest pain and exposure of the muscle layer fibers. A CT scan of the chest revealed a small leakage of carbon dioxide, which had been used for insufflation during the procedure. The patient had an otherwise uneventful recovery.
To refer a patient to the UH Digestive Health Institute for ESD in the esophagus, stomach or colon, contact John Dumot, DO, Director, UH Digestive Health Institute; Professor of Medicine, Case Western Reserve University School of Medicine at 216-593-1305 or John.Dumot@UHhospitals.org or Amitabh Chak, MD, Medical Director, Advanced Technology & Innovation Center, UH Digestive Health Institute; Professor of Medicine, Case Western Reserve University School of Medicine at 216-844-3217 or Amitabh.Chak@UHhospitals.org.
Tags:


