Radiation Therapies to Target and Kill Prostate Cancer Cells
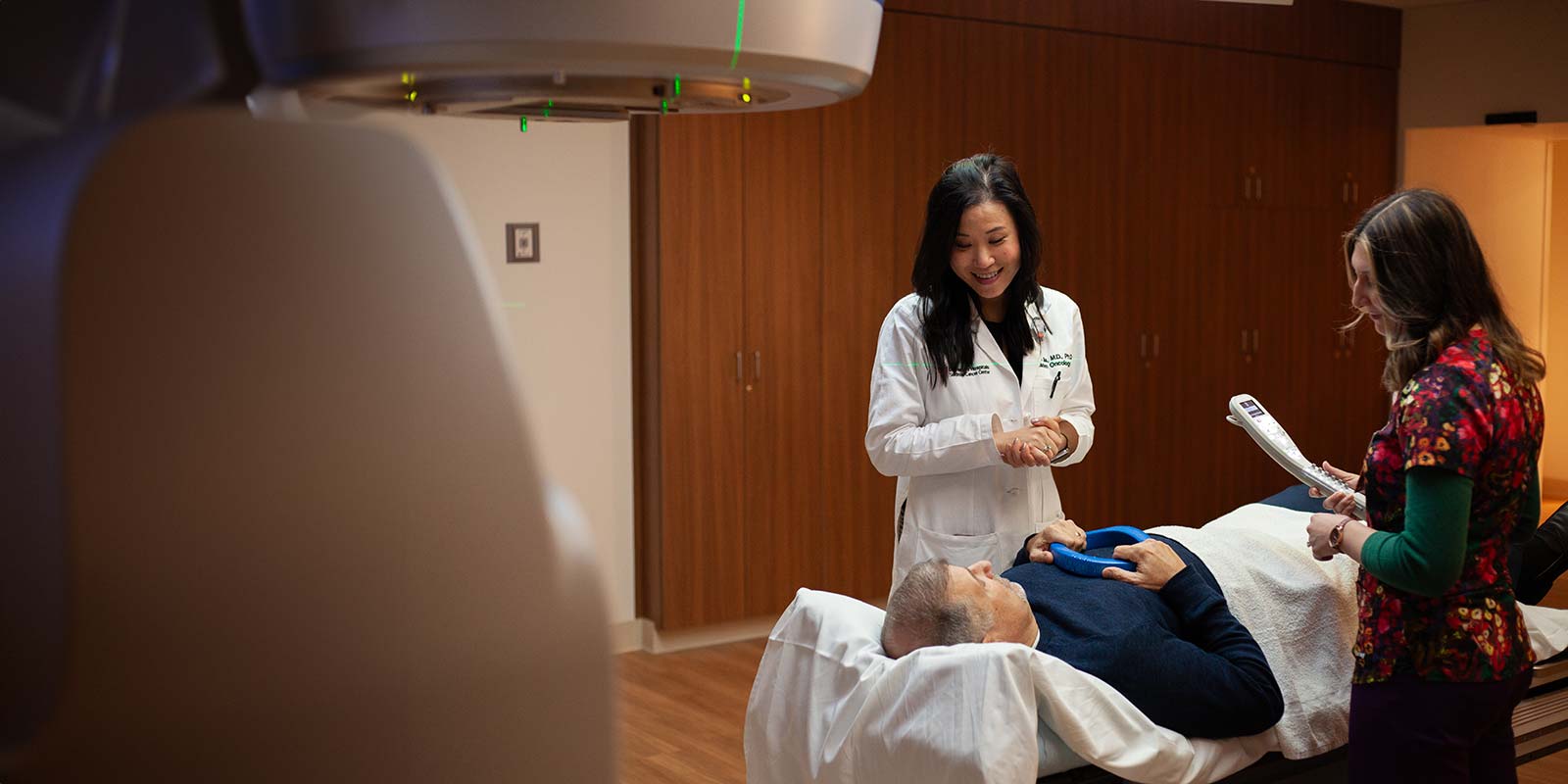
Radiation therapy uses high-energy radiation to destroy cancer cells in a precise manner and is a cornerstone of prostate cancer management across various stages of the disease. In early-stage localized prostate cancer (cancer that has not spread to other part of the body), it is used to precisely kill cancer cells while preserving healthy tissue. In some case, radiation is the only treatment option needed.
In more advanced prostate cancer cases, radiation is often combined with medical therapies (for example, androgen deprivation therapy) or surgery to improve treatment effectiveness. Radiation therapy is also used to manage recurrent disease after prior surgery. Radiation therapies are provided by cancer specialists called radiation oncologists.
Your health is important. Get expert care.
If you have been diagnosed with prostate cancer, call 216-844-3951 today to schedule an appointment with a prostate cancer expert. We offer both initial consults and second opinion appointments.
Types of Radiation Therapy
There are two main types of radiation therapy: external and internal.
External Beam Radiation Therapy
External radiation therapy uses focused beams of energy to kill cancer cells and is often the first treatment for low-grade cancers that are contained within the prostate gland. It may also be used along with other therapies for cancers that have spread into nearby tissues. The therapy is a non-invasive, painless method to kill cancer cells.
University Hospitals offers several highly advanced forms of EBRT treatment options, including:
- Proton Beam Radiation Therapy
-
Proton therapy uses robotic technology and an image guidance system to deliver a highly targeted beam of radiation to the tumor, with fewer side effects and less damage to healthy tissue. It also has the ability to deliver higher, more focused doses of energy to tumors that are difficult to reach or in areas prone to radiation damage.
- Intensity Modulated Radiation Therapy (IMRT)
-
For this type of radiation therapy, doctors use advanced computer technology to adjust and shape the beam so radiation to match the exact size and shape of your prostate. This allows us to deliver a high dose of radiation directly to the cancer while minimizing exposure of nearby healthy tissues, like the bladder and rectum.
- Image-guided radiation therapy (IGRT)
-
This method of radiation therapy uses special equipment that is equipped with sophisticated imaging capabilities that allow the doctor to clearly view the tumor before and during treatment. The images can help to improve the accuracy of the radiation beam and more precisely target the tumor while avoiding healthy surrounding tissue.
- Stereotactic body radiation therapy (SBRT)
-
Using advanced image-guidance techniques, SBRT allows extremely precise, high doses of radiation to be delivered safely to kill cancer. Because SBRT delivers larger doses of radiation than conventional radiation therapy, fewer treatments are needed. These treatment may be given over a few days instead of weeks.
SBRT technologies we use to treat prostate cancer include:
- Varian Edge Radiation Therapy: The Varian Edge radiation beam target tumors with a high degree of precision, sparing healthy tissue and causing fewer side effects than conventional radiation therapy. This breakthrough radiotherapy utilizes the latest in real-time tumor tracking technology and motion management capabilities to optimize patient safety, comfort and quality of life.
- Varian Ethos Adaptive Radiotherapy: Varian Ethos adaptive radiotherapy allows treatment to be adjusted according to changes in the size, shape or location of the tumor to precisely target the cancer while protecting surrounding healthy tissue. The technology can be particularly helpful in treating cancers that respond well to very high doses of radiation, such as prostate cancer. In observing changes in the prostate gland’s exact position relative to nearby organs on the day of treatment, Varian Ethos allows the highest dose of radiation to be precisely and safely delivered to the cancer.
Internal Radiation Therapy (Brachytherapy)
Internal radiation therapy treats cancer by introducing a radioactive material into the body. The main internal radiation therapies used in the treatment of prostate cancer are brachytherapy and radionuclide therapy.
Brachytherapy
In brachytherapy, a radioactive material is implanted directly into the body, inside or near the tumor. Brachytherapy may be the only treatment needed if the prostate tumor is small and contained within the gland. More often, it is combined with other therapies as part of a total treatment plan.
There are two main types of brachytherapy for prostate cancer: low dose rate (LDR) brachytherapy and high dose rate (HDR) brachytherapy. Your care team will explain these options to you and determine which type of brachytherapy is best for you and why.
During LDR brachytherapy, radioactive pellets or seeds are implanted into the prostate through a thin, hollow needle. The doctor uses advanced imaging technology to guide the needle, ensuring the pellets are accurately placed in or near the tumor. Patients are usually sedated while the device is positioned to help them remain still and minimize discomfort.
With LDR, the radioactive material left in place for several hours or several days, continuously giving off low doses of radiation to the tumor. Because the radiation from the seeds only travels a very short distance, there is minimal damage to nearby healthy tissues. Although the radioactive material is inside your body, there is some risk of exposure to other people so patients usually remain in the hospital with limited visitation during treatment. After a pre-determined amount of time, the radioactive material is removed from your body.
For HDR brachytherapy, a very high dose of radioactive material is placed inside or near the tumor for a short time - usually no longer than 20 minutes. The doctor uses advanced imaging technology to accurately position one or more catheters (thin flexible tubes) containing the radioactive material in or near the tumor.
After a pre-determined amount of time, the radioactive material is removed. Patients may undergo one or two sessions a day over a number of days or weeks. HDR brachytherapy is typically an outpatient procedure, which means patients do not have to stay in the hospital during treatment.
Radionuclide Therapy
Radionuclide therapy uses radioactive drugs to target and destroy cancer cells. Taken by mouth or intravenous injection, radionuclide therapy is a systemic treatment, meaning the medication flows through the bloodstream and affects the entire body. However, unlike chemotherapy, radionuclide therapy targets cancer cells, decreasing potential side effects.

SpaceOAR™ Hydrogel
We are pleased to offer our patients SpaceOAR™ Hydrogel – an FDA-cleared procedure to help minimize urinary, sexual and bowel side effects for patients undergoing any type of prostate cancer radiation therapy. University Hospitals was designated the first SpaceOAR Hydrogel Center of Excellence in the world.
SpaceOAR Hydrogel is a water-based synthetic material that is injected into the space between the prostate and the rectum. The procedure is done under local, regional or general anesthesia before radiation treatment begins. Once in place, the gel hardens to create a temporary barrier between the rectum and the prostate, reducing the radiation dose to the rectum during treatment.
The barrier created by the SpaceOAR gel will last for about 3 months and, after 6 months, will be naturally absorbed by the body and removed in your urine.
Side Effects of Radiation Therapies
Regardless of the delivery method, most radiation therapies for prostate cancer can cause significant side effects. The severity of side effects and the length of time they persist will be different for each man. Often they will resolve over time but, for some men, the effects can be permanent. The most common side effects of radiation therapy to the prostate include:
- Fatigue
- Bowel problems, including diarrhea and blood in the stool.
- Urinary problems, including frequency, urgency and weak urinary stream; less commonly, blood in the urine and burning urination; and very rarely, incontinence.
- Erectile dysfunction
Our multidisciplinary team of experts will work with each patient to manage and provide follow-up care for any side effects that may occur with radiation therapy.
Advanced Technologies to Minimize the Side Effects of Radiation Therapy
At University Hospitals, we use fiducial markers to further improve precision and safety of radiation therapy for prostate cancer. Fiducial markers are small gold markers implanted in the prostate to allow more accurate targeting of the prostate during imaging and treatment, ensuring the radiation dose is delivered precisely to the tumor. We also offer a wide range of multidisciplinary follow-up therapies and treatments to help patients manage, and in some cases, resolve side effects of radiation therapy.


