Information on Enlarged Vestibular Aqueduct Syndrome (EVA)
Many unanswered questions remain about the causes, diagnosis, clinical course and treatment of patients with EVA. Information is available through our Health Library or with the following diagrams and more detailed EVA information to give a greater understanding of how EVA occurs and what may trigger EVA.
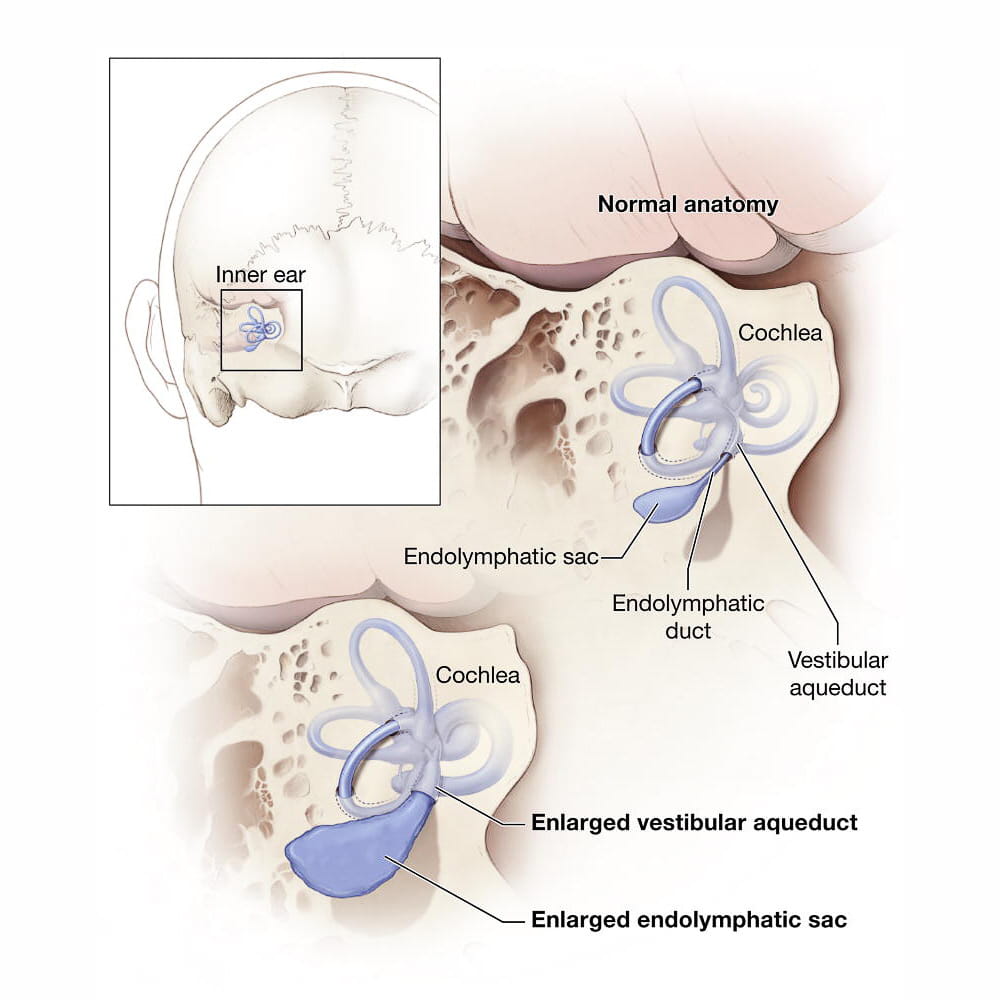
Structure of the Inner Ear
A vestibular aqueduct is a small, bony canal with the temporal bone of the skull (behind the ear) that connects the inner ear to a nearby balloon-shaped structure called the endolymphatic sac. The inner ear structures consist of separate hearing and balance organs, known as the cochlea and vestibular apparatus, respectively. The cochlea, vestibular organ and nerves that send signals to the brain are responsible for processing sound transmission and contributing to the body’s sense of balance. Anatomic abnormalities of these structures may contribute to hearing loss, balance disturbances, or both.
Definition of EVA
A vestibular aqueduct that is larger than 1 mm is considered enlarged. The enlarged vestibular aqueduct (EVA) may be a sign of corresponding enlargement of the endolymphatic duct (which runs through the vestibular aqueduct) and the endolymphatic sac. Abnormalities in these structures contribute to sensorineural hearing loss by a mechanism that is not entirely understood. The fluids within the endolymphatic duct and sac must remain in careful balance such that any changes, however subtle, may precipitate a hearing loss.
Pendred Syndrome and EVA
EVA may be a component of Pendred syndrome which is characterized by hearing loss due to EVA and thyroid disease, among other things. According to a study by the National Institute on Deafness and Other Communication Disorders (NICDC), approximately a quarter of people with EVA and hearing loss have Pendred syndrome. The hearing loss associated with Pendred syndrome is more likely to be progressive, meaning there is a reasonable likelihood the hearing loss may progress and become more severe, perhaps even resulting in deafness.
Hearing Loss May Affect Balance Center in the Ear
Given the close anatomic relationship between the hearing and balance centers in the inner ear and their connection to the endolymphatic sac through the vestibular aqueduct, it is no surprise that children with hearing loss associated with EVA may also have problems with their balance. Fortunately, the brain is very adept at compensating for such an abnormality so these balance difficulties are typically transient and mild. If balance disturbances are more problematic, specific vestibular testing with focused vestibular rehabilitation may be required.
Causes of EVA are Likely Multifactorial
The exact cause of EVA is unknown but is likely multifactorial. The most well-known cause of EVA and hearing loss is a gene mutation, known as SLC26A4 (previously known as the PDS gene). Two mutations in the SLC26A4 gene can result in Pendred syndrome and other factors, genetic or environmental, may also lead to EVA.
Investigation into a suspected hearing loss typically involves confirmatory hearing testing, often with age-appropriate audiometry and, possibly auditory brainstem response (ABR) testing. Once a sensorineural hearing loss has been confirmed, imaging is often obtained to evaluate the anatomy of the inner ear. This is perhaps more important in the setting of unilateral or sudden hearing loss and would consist of magnetic resonance imaging (MRI), computed tomography (CT) scanning, or both. Although most imaging studies in this setting are normal, the most common finding on an abnormal CT is EVA.
Managing and Treating EVA

Surgical considerations such as surgical procedures to drain liquid out of the endolymphatic duct and sac or to remove the endolymphatic duct and sac are not only ineffective in treating EVA, it can be harmful. Research has shown conclusively that surgeries such as these can actually destroy hearing.
Certain activities have been demonstrated to precipitate a decrease in an EVA patient’s hearing and include contact sports where the participant could sustain a head injury, and activities where barotrauma is more likely. Activities such as contact sports, cycling, or skiing should be undertaken with protective headgear or avoided altogether. Any situations that can lead to barotrauma or rapid changes in air pressure such as scuba diving or hyperbaric oxygen treatments should be carefully avoided because of their risk of sudden worsening of hearing loss. In addition, added pressure changes with air travel have also been reported to cause hearing loss in EVA patients. This is a rare event in commercial aircraft with pressurized cabins and this risk may be minimized by preemptively taking a nasal decongestant, particularly if there is sinus or nasal congestion.
Early Diagnosis Reduces EVA’s Impact
Identifying hearing loss as early as possible is the best way to reduce EVA’s impact. The earlier hearing loss is identified in children, the sooner they can develop skills that will help them learn and communicate with others. Children with permanent and progressive hearing loss, which often is linked with EVA, will benefit from learning other forms of communication, such as sign language or cued speech, or using assistive devices, such as a hearing aid or cochlear implant.


