Infective Endocarditis Prophylaxis

Infective Endocarditis
Also known as bacterial endocarditis or subacute bacterial endocarditis (SBE), infective endocarditis (IE) occurs when blood-borne bacteria infect the endocardial lining of the heart and/or the heart valves. If not detected and treated, heart valves can be damaged or even destroyed.
There are multiple ways that bacteria that are commonly found on the skin, in the oropharynx or elsewhere in the body can enter the bloodstream where they can multiply and cause bacteremia. Certain strains of bacteria lodge on susceptible portions of the heart – typically on damaged areas or on foreign material in the heart. Because these are risk factors, some groups of patients are more susceptible to IE than others. It is important to recognize that the most common cause of transient bacteremia is frequent exposure to bacteria during daily activities including chewing and brushing your teeth. Thus, baseline poor dental hygiene is a significant contributing factor, making good oral health and hygiene, including regular dental visits, important in all at-risk patients. Injuries or invasive procedures, such as certain surgeries or dental procedures, have also been identified as risk factors for the development of IE.
Often IE smolders, creating nonspecific symptoms which hinder diagnosis until the amount of bacteria in the blood reaches critical levels, producing high fever and more fulminant symptoms. Diagnosis is often further hindered by administration of antibiotics before blood cultures are drawn, eliminating bacteria in the blood, but not in the heart.
Detecting Infective Endocarditis
Should a patient have signs or symptoms that suggest possible endocarditis, they should see a doctor immediately and have blood cultures and other relevant tests done before antibiotics are started. This will allow for accurate diagnosis and also help direct therapy.
Prophylaxis: New Guidelines
In recent years, the Endocarditis Committee of the American Heart Association conducted an extensive review, determining which procedures are most likely to cause endocarditis, and released new guidelines indicating which patients should receive SBE prophylaxis. In comparison to the old guidelines, the revised guidelines suggest that fewer patients need to receive SBE prophylaxis.
Patients at highest risk
The Endocarditis Committee of the American Heart Association now recommends antibiotic prophylaxis only for those patients at highest risk for an adverse outcome.
These patients include:
- Those who have a prosthetic cardiac valve or a cardiac valve repair done with prosthetic material
- Those who have had previous endocarditis
- Those with the following particular congenital conditions:
– Unrepaired cyanotic congenital heart disease, including those with palliative shunts and conduits
– A congenital heart defect that is completely repaired with prosthetic material or a prosthetic device, placed by either surgery or catheter, for the first six months after the procedure
– Congenital heart disease that is repaired but with residual defects (persistent leaks or abnormal flow) at or adjacent to the site of a prosthetic patch or device
- Those who have had a cardiac transplant and have developed cardiac valve abnormalities
Patient groups no longer requiring antibiotic prophylaxis
Some patient groups included previously were found not to require antibiotic prophylaxis.
Among these are patients who have:
- Congenital heart defects not listed above (including bicuspid aortic valve)
- Hypertrophic cardiomyopathy
- Coronary artery bypass graft surgery
- Coronary artery stents
Changes in guidelines do not, however, change the fact that some patients are inherently more at risk than others, even if excluded from the current groups for whom prophylaxis is recommended. The judgment of each patient’s cardiologist, based upon their specific case, should be the deciding factor regarding antibiotic administration.
Procedures that do not require antibiotic prophylaxis
The Endocarditis Committee of the American Heart Association and national and international experts on IE determined that there is no conclusive evidence that certain specific dental procedures create IE, nor is there evidence that gastrointestinal or genitourinary tract procedures cause IE, even in the highest-risk patients.
Procedures which do not require antibiotic prophylaxis include:
- Gastrointestinal procedures, even in the highest-risk patients
- Genitourinary procedures, even in the highest-risk patients
- Any dental procedures other than in the highest-risk patients
- The following dental procedures even in the highest-risk patients:
- Routine injections of anesthetic through noninfected tissue
- Dental radiography
- Placing prosthodontic or orthodontic appliances
- Adjusting orthodontic appliances
- Placing orthodontic brackets
- Deciduous tooth loss
- Lip or oral mucosa trauma with bleeding
Antibiotic prophylaxis for highest-risk patients
Procedures where antibiotic prophylaxis is recommended
For highest-risk patients, prophylaxis is appropriate for all dental procedures that involve:
- Manipulation of gingival tissue
- Manipulation of the periapical region of teeth
- Perforation of the oral mucosa
- Trauma to the lips or oral mucosa with bleeding
Antibiotic prophylaxis is also recommended for highest-risk patients in the case of an invasive procedure involving incision or biopsy of the respiratory mucosa, such as:
- Tonsillectomy
- Adenoidectomy
- Bronchoscopy only in the case of incision of the mucosa
- Treatment of an established infection, i.e., drainage of an abscess or empyema
In highest-risk patients, prophylaxis is also recommended for procedures involving infected skin, skin structures or musculoskeletal tissue.
Antibiotic Prophylactic Regimens for Dental Procedures
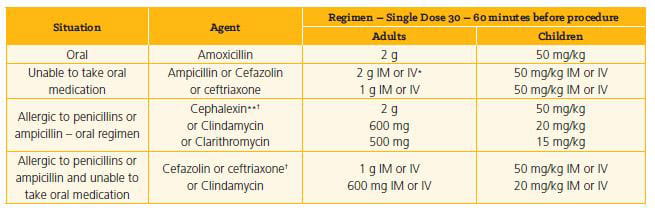
*IM – intramuscular; IV – intravenous
**Or other first- or second-generation oral cephalosporin in equivalent adult or pediatric dosage
† Cephalosporins should not be used in an individual with a history of anaphylaxis, angioedema or urticaria with penicillins or ampicillin.
Source: American Heart Association
Specific situations and circumstances – patients already receiving antibiotics
If a patient is already receiving long-term antibiotic therapy, it is prudent to select an antibiotic from a different class rather than to increase the dosage of the current antibiotic. For example, antibiotic regimens used to prevent the recurrence of acute rheumatic fever are administered in dosages lower than those recommended for the prevention of IE.
Reference:
Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, et al. Circulation 2007; 116:1736 – 1754.
Contact Us
Physician-to-Physician Consultation Line, 216-UH4-ADOC (216-844-2362)
Physician Access Line, 216-UH4-PEDS (216-844-7337)
(Patient transfers, admissions referrals, emergency department referrals, appointments)


