Pituitary Tumors
At UH Seidman Cancer Center, our team of fellowship-trained cancer doctors and surgeons provides leading-edge diagnostics, advanced techniques and targeted therapies for treating pituitary tumors.
UH Seidman Cancer Center is part of the National Cancer Institute-designated Case Comprehensive Cancer Center at Case Western Reserve University School of Medicine, part of an elite group of 53 comprehensive cancer hospitals nationwide. Our nationally recognized cancer program provides expertise in both routine and very complex care.
Your health is important. Make an appointment today.
Offering in-person, video and telephone visits. Call todayto see which option is right for you. 216-844-3951
Learn more about virtual visits
What Are Pituitary Tumors?
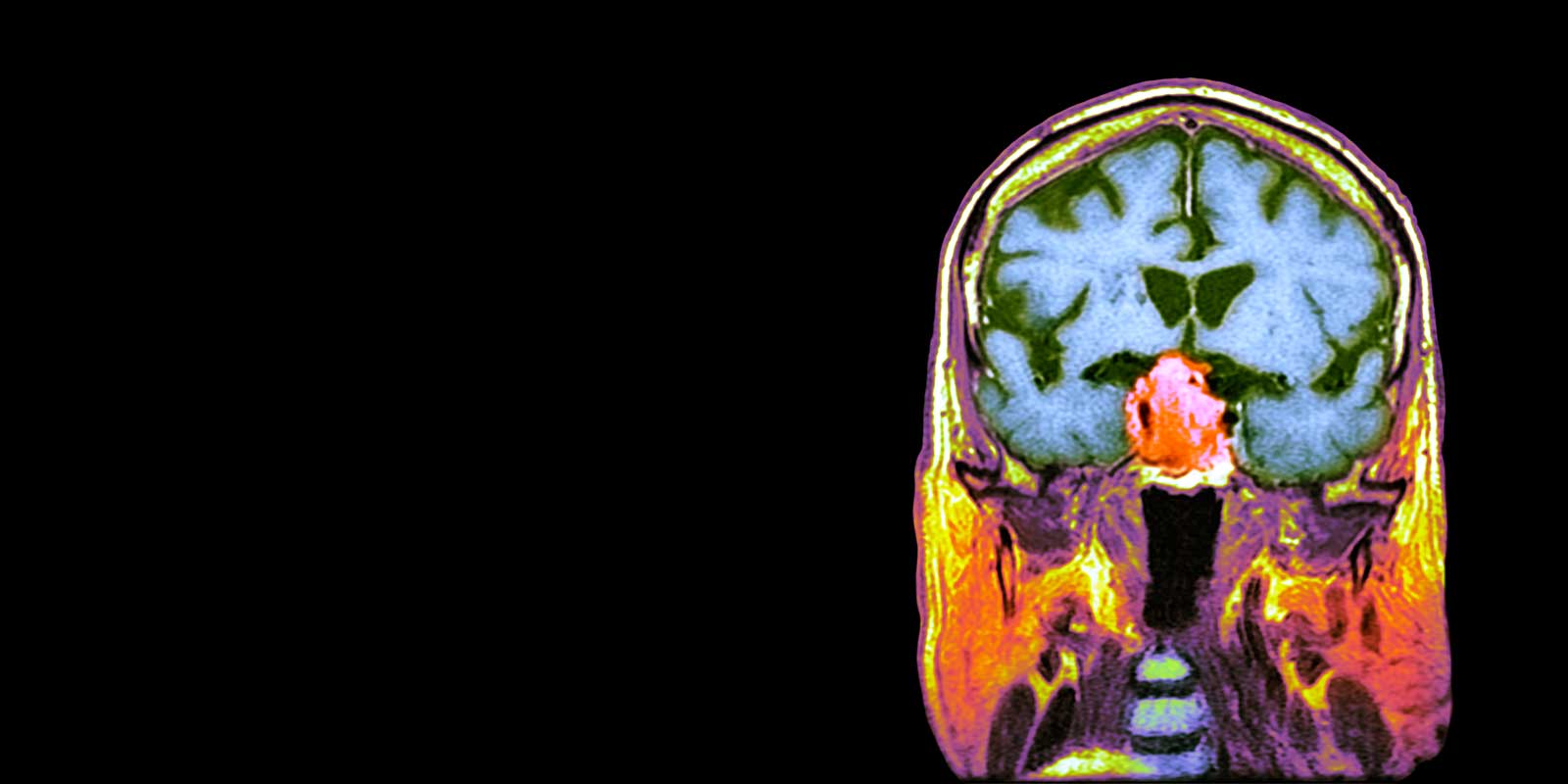
A pituitary tumor is a growth of abnormal cells in the pituitary gland, a pea-sized organ located at the base of the brain just behind the eyes. Sometimes referred to as the “master endocrine gland” because it produces hormones that affect the way many parts of the body work, the pituitary gland also controls hormones made by other glands in the body.
Nearly all pituitary tumors are benign (noncancerous) glandular tumors called pituitary adenomas. Nevertheless, benign pituitary tumors can cause serious health issue due to their location in the brain, their ability to spread to nearby tissues (i.e., the skull and the sinuses) and their tendency to produce excess hormones. Microadenomas are pituitary adenomas that are smaller than 1 centimeter, while those larger than 1 centimeter are called macroadenomas. The majority of pituitary adenomas are microadenomas.
Cancerous pituitary tumors, called pituitary carcinomas, are extremely rare. In fact, only a few hundred cases of pituitary carcinoma have ever been recorded in the U.S.
Pituitary tumors may be either non-functioning or functioning:
- Non-functioning pituitary tumors do not produce extra amounts of hormones.
- Functioning pituitary tumors secrete more than the normal amount of one or more hormones. The majority of pituitary tumors are functioning tumors. Extra hormones produced by pituitary tumors often cause certain signs or symptoms of disease.
What Are Pituitary Tumor Symptoms?
Signs and symptoms of pituitary adenomas depend on whether the tumors are functioning (hormone-producing) or non-functioning, among other factors. Some pituitary tumors may not cause any signs or symptoms.
Signs and Symptoms of Non-Functioning Pituitary Tumors
A non-functioning pituitary tumor can press on or damage parts of the pituitary gland, causing it to stop producing one or more hormones. Such tumors can cause the following symptoms:
- Headache
- Loss of some vision
- Loss of body hair
- In women, less frequent or no menstrual periods or no breast milk production
- In men, loss of facial hair, growth of breast tissue and impotence
- Lower sex drive in both men and women
- Slowed growth and sexual development in children
Signs and Symptoms of Functioning Pituitary Tumors
Signs and symptoms of functioning pituitary tumors usually are associated with whatever extra hormone or hormones are being made.
- Signs and Symptoms of Excess Prolactin:
-
- Headache
- Loss of some vision
- Less frequent or no menstrual periods or else menstrual periods with a very light flow
- Difficulty or inability to become pregnant
- Impotence in men
- Lower sex drive in both men and women
- Breast milk production in women who are not pregnant or breastfeeding
- Signs and Symptoms of Excess Adrenocorticotropic Hormone (ACTH)
-
- Headache
- Loss of some vision
- Weight gain in the face, neck and body trunk
- Thin arms and/or legs
- A lump of fat on the back of the neck
- Thin skin on the abdomen or chest that may have pink or purple stretch marks
- Easy bruising
- Growth of fine hair on the face, arms or upper back
- Bones that break easily
- Anxiety, irritability and depression
- Signs and Symptoms of Excess Growth Hormone:
-
- In adults, acromegaly (abnormal growth of the bones in the face, hands and feet)
- In children, the body may grow abnormally taller and larger
- Headache
- Loss of some vision
- Numbness or tingling in the hands and fingers
- Snoring or pauses in breathing during sleep
- Joint pain
- Excessive sweating
- Body dysmorphic disorder (concern about a perceived flaw in one or more parts of a person’s own body)
- Signs and Symptoms of Excess Thyroid-Stimulating Hormone:
-
- Irregular heartbeat
- Shakiness
- Weight loss
- Difficulty sleeping
- Frequent bowel movements
- Sweating
- Other General Signs and Symptoms of Pituitary Tumors:
-
- Nausea and vomiting
- Confusion
- Dizziness
- Seizures
- Cerebrospinal fluid leaking into the nose

What Causes Pituitary Gland Tumors?
The cause of the abnormal, unchecked cell growth in the pituitary gland that leads to tumors is unknown. A small percentage of pituitary tumor cases run in families, but most do not have a hereditary basis. Nevertheless, medical scientists suspect that genetic alterations play an important role in the development of pituitary tumors. Individuals with a family history of certain hereditary conditions, including multiple endocrine neoplasia type 1 (MEN 1), have an increased risk of developing a pituitary tumor.
Pituitary Gland Tumor Survival Rate
In general, having a benign pituitary (pituitary adenoma) does not shorten life expectancy if the tumor is treated properly and if the patient undergoes the appropriate hormone replacement therapy.
A 5-year survival rate indicates what percent of people live at least five years after a tumor is found. In the case of pituitary adenomas, the 5-year survival rate is approximately 97%. Note that survival rates depend on the type of tumor, the person’s age and other factors.
Treatment for Pituitary Tumors
The UH Seidman Cancer Center team works closely with specialists from University Hospitals Neurological Institute’s Brain Tumor and Neuro-Oncology Center and endocrinologists at The University Hospitals Division of Clinical & Molecular Endocrinology to design treatments customized to the needs of pituitary tumor patients.
Surgery is the primary treatment option for pituitary adenomas. The most common pituitary tumor surgery procedures are:
- Transsphenoidal Surgery: The most common surgical method to remove pituitary tumors, transsphenoidal surgery is done through the spheroid sinus, which is located in the skull behind the nasal passages and below the brain. Although more invasive than endoscopic procedures, this surgery does not involve contact with the brain, has fewer side effects and does not leave a visible scar.
- Endoscopic Surgery: In this minimally invasive procedure, the neurosurgeon inserts a thin fiber-optic tube fitted with a tiny camera through a small incision in the nose, allowing the neurosurgeon to see and reach the pituitary gland and remove the tumor.
- Craniotomy: This procedure may be used in the removal of larger tumors. In a craniotomy, the neurosurgeon operates through an opening made in the front of the skull.
In addition to surgery, patients with benign pituitary tumors may also receive:
- Radiation therapy: Radiation therapy may be employed following pituitary tumor surgery to prevent regrowth of the tumor. In addition, radiation therapy may also be used as the sole treatment if the pituitary tumor cannot be extracted via surgery or if the tumor recurs after surgery. We also offer stereotactic radiosurgery, a form of radiation therapy in which high-power energy is focused on a small area of the body. In particular, we treat patients using the Varian Edge™ and Gamma Knife® radiosurgery systems.
- Drug Therapy: Drugs may be prescribed to stop a functioning pituitary tumor from producing excessive amounts of hormones.

Innovative Research Leads to New Opportunities in Care
University Hospitals is an affiliate of Case Western Reserve University School of Medicine, a nationally recognized leader in clinical research. UH Seidman Cancer Center currently conducts a number of clinical trials for patients with brain and skull base tumors, giving patients access to new and innovative therapies and treatment options.
Why Choose UH Seidman Cancer Center for Pituitary Tumor Treatment?
Part of the NCI-designated Case Comprehensive Cancer Center at Case Western Reserve University School of Medicine – one of an elite group of 53 comprehensive cancer hospitals nationwide.
The first stereotactic radiosurgery suite in Ohio to offer Gamma Knife® technology for malignant and benign brain tumors
The first hospital in Ohio to offer proton therapy – an innovative, technologically advanced cancer treatment
Patient-Centered Diagnostics and Treatment
We employ a multidisciplinary approach in the treatment or pituitary and other types of brain tumors. This means all our cancer doctors, nurses and support staff collaborate and coordinate your care. UH Seidman Cancer Center puts the patient at the center of a compassionate, highly trained team so they can feel confident with each step of the diagnosis, treatment and care management process. Our team of experts includes:
- Genetic counselors
- Medical geneticists
- Medical oncologists
- Nurse navigators
- Nurse practitioners
- Pathologists
- Radiation oncologists
- Radiologists
- Social workers
- Surgical oncologists



