Primary Central Nervous System Lymphoma Treatment
General Information About Primary CNS Lymphoma
Key Points
- Primary central nervous system (CNS) lymphoma is a disease in which malignant (cancer) cells form in the lymph tissue of the brain and/or spinal cord.
- Having a weakened immune system may increase the risk of developing primary CNS lymphoma.
- Signs and symptoms of primary CNS lymphoma may include nausea and vomiting or seizures.
- Tests that examine the eyes, brain, and spinal cord are used to diagnose primary CNS lymphoma.
- Certain factors affect prognosis (chance of recovery) and treatment options.
Primary central nervous system (CNS) lymphoma is a disease in which malignant (cancer) cells form in the lymph tissue of the brain and/or spinal cord.
Lymphoma is a disease in which malignant (cancer) cells form in the lymph system. The lymph system is part of the immune system and is made up of the lymph, lymph vessels, lymph nodes, spleen, thymus, tonsils, and bone marrow. Lymphocytes (carried in the lymph) travel in and out of the central nervous system (CNS). It is thought that some of these lymphocytes become malignant and cause lymphoma to form in the CNS. Primary CNS lymphoma can start in the brain, spinal cord, or meninges (the layers that form the outer covering of the brain). Because the eye is so close to the brain, primary CNS lymphoma can also start in the eye (called ocular lymphoma).
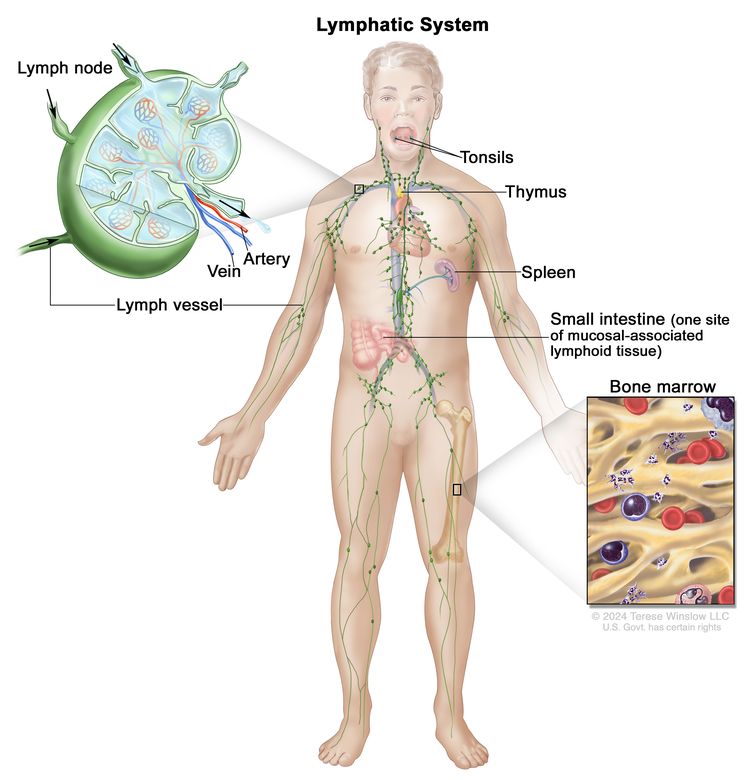
Anatomy of the lymph system, showing the lymph vessels and lymph organs including lymph nodes, tonsils, thymus, spleen, and bone marrow. Lymph (clear fluid) and lymphocytes travel through the lymph vessels and into the lymph nodes where the lymphocytes destroy harmful substances. The lymph enters the blood through a large vein near the heart.
Having a weakened immune system may increase the risk of developing primary CNS lymphoma.
Anything that increases a person's chance of getting a disease is called a risk factor. Not every person with one or more of these risk factors will develop primary CNS lymphoma, and it will develop in people who don't have any known risk factors. Talk with your doctor if you think you may be at risk.
Primary CNS lymphoma may occur in patients who have HIV, AIDS, Epstein-Barr virus, or other disorders of the immune system, or who have had an organ transplant. For more information about lymphoma in patients with AIDS, see AIDS-Related Lymphoma Treatment.
Signs and symptoms of primary CNS lymphoma may include nausea and vomiting or seizures.
These and other signs and symptoms may be caused by primary CNS lymphoma or by other conditions. Check with your doctor if you have any of the following:
Tests that examine the eyes, brain, and spinal cord are used to diagnose primary CNS lymphoma.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
- Neurological exam: A series of questions and tests to check the brain, spinal cord, and nerve function. The exam checks a person’s mental status, coordination, ability to walk normally, and how well the muscles, senses, and reflexes work. This may also be called a neuro exam or a neurologic exam.
- Eye exam with dilated pupil: An exam of the eye in which the pupil is dilated (enlarged) with medicated eye drops to allow the doctor to look through the lens and pupil to the retina. The inside of the eye, including the retina and the optic nerve, is checked. Pictures may be taken over time to keep track of changes in the size of the tumor. There are several types of eye exams:
- Ophthalmoscopy: An exam of the inside of the back of the eye to check the retina and optic nerve using a small magnifying lens and a light.
- Slit-lamp biomicroscopy: An exam of the inside of the eye to check the retina, optic nerve, and other parts of the eye using a strong beam of light and a microscope.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the brain and spinal cord. A substance called gadolinium is injected into the patient through a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture. This procedure is also called nuclear magnetic resonance imaging (NMRI).
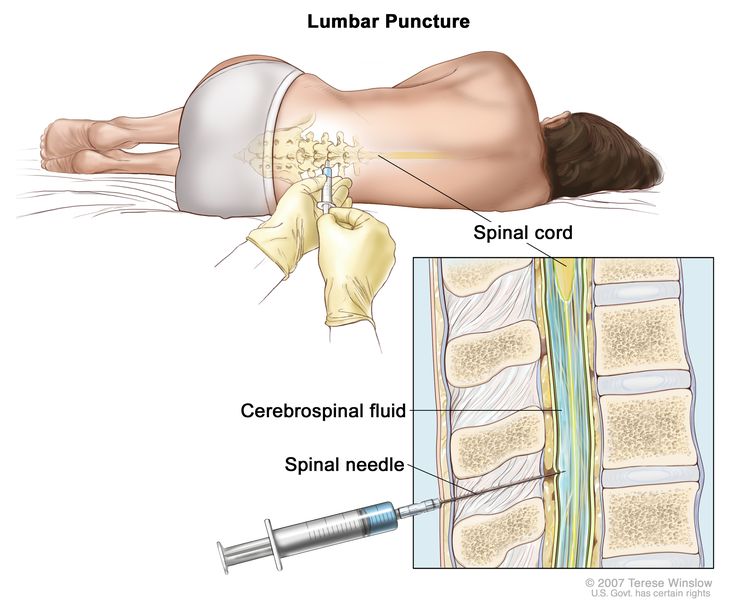
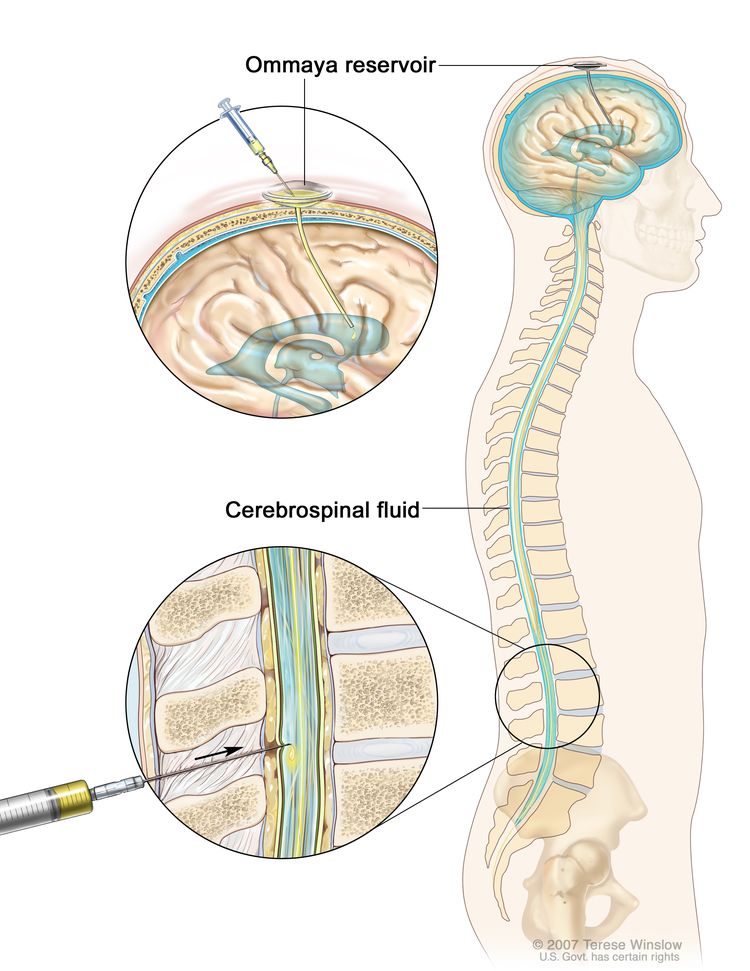
- Lumbar puncture: A procedure used to collect cerebrospinal fluid (CSF) from the spinal column. This is done by placing a needle between two bones in the spine and into the CSF around the spinal cord and removing a sample of the fluid. The sample of CSF is checked under a microscope for signs of tumor cells. The sample may also be checked for the amounts of protein and glucose. A higher than normal amount of protein or lower than normal amount of glucose may be a sign of a tumor. This procedure is also called an LP or spinal tap.
 Enlarge
Enlarge
Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing. - Stereotactic biopsy: A biopsy procedure that uses a computer and a 3-dimensional (3-D) scanning device to find a tumor site and guide the removal of tissue so it can be viewed under a microscope to check for signs of cancer.
The following tests may be done on the samples of tissue that are removed:
- Flow cytometry: A laboratory test that measures the number of cells in a sample, the percentage of live cells in a sample, and certain characteristics of the cells, such as size, shape, and the presence of tumor (or other) markers on the cell surface. The cells from a sample of a patient’s blood, bone marrow, or other tissue are stained with a fluorescent dye, placed in a fluid, and then passed one at a time through a beam of light. The test results are based on how the cells that were stained with the fluorescent dye react to the beam of light. This test is used to help diagnose and manage certain types of cancers, such as leukemia and lymphoma.
- Immunohistochemistry: A laboratory test that uses antibodies to check for certain antigens (markers) in a sample of a patient’s tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type of cancer.
- Cytogenetic analysis: A laboratory test in which the chromosomes of cells in a sample of blood or bone marrow are counted and checked for any changes, such as broken, missing, rearranged, or extra chromosomes. Changes in certain chromosomes may be a sign of cancer. Cytogenetic analysis is used to help diagnose cancer, plan treatment, or find out how well treatment is working.
- FISH (fluorescence in situ hybridization): A laboratory test used to look at and count genes or chromosomes in cells and tissues. Pieces of DNA that contain fluorescent dyes are made in the laboratory and added to a sample of a patient’s cells or tissues. When these dyed pieces of DNA attach to certain genes or areas of chromosomes in the sample, they light up when viewed under a fluorescent microscope. The FISH test is used to help diagnose cancer and help plan treatment.
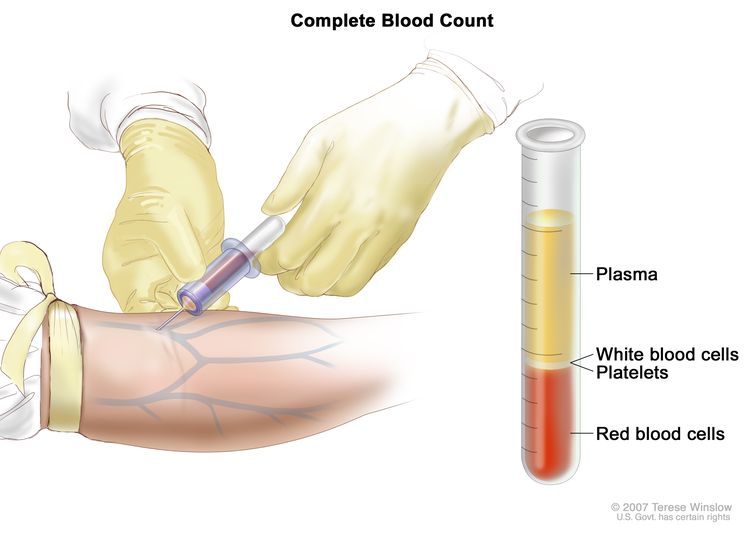
- Complete blood count (CBC) with differential: A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells and platelets.
- The number and type of white blood cells.
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the blood sample made up of red blood cells.
 Enlarge
Enlarge
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis depends on the following:
- Whether the patient has HIV.
- The patient's age and general health.
- Whether the tumor is in the central nervous system, eye, or both.
- The level of certain substances in the blood and cerebrospinal fluid (CSF).
Treatment options depend on the following:
- Whether the tumor is in the central nervous system, eye, or both.
- The patient's age and general health.
- Whether the cancer has just been diagnosed or has recurred (come back).
Treatment of primary CNS lymphoma works best when the tumor has not spread outside the cerebrum (the largest part of the brain) and the patient is younger than 60 years, able to carry out most daily activities, and does not have AIDS or other diseases that weaken the immune system.
Staging Primary CNS Lymphoma
Key Points
- After primary central nervous system (CNS) lymphoma has been diagnosed, tests are done to find out if cancer cells have spread within the brain and spinal cord or to the eye.
- There is no standard staging system for primary CNS lymphoma.
- Primary CNS lymphoma often recurs (comes back) after it has been treated.
After primary central nervous system (CNS) lymphoma has been diagnosed, tests are done to find out if cancer cells have spread within the brain and spinal cord or to the eye.
Primary CNS lymphoma usually does not spread beyond the central nervous system or the eye. The process used to find out if cancer has spread is called staging. There is no standard system for staging primary CNS lymphoma.
The following tests and procedures may be used to help plan treatment:
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. A PET scan and CT scan may be done at the same time. This is called a PET-CT.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
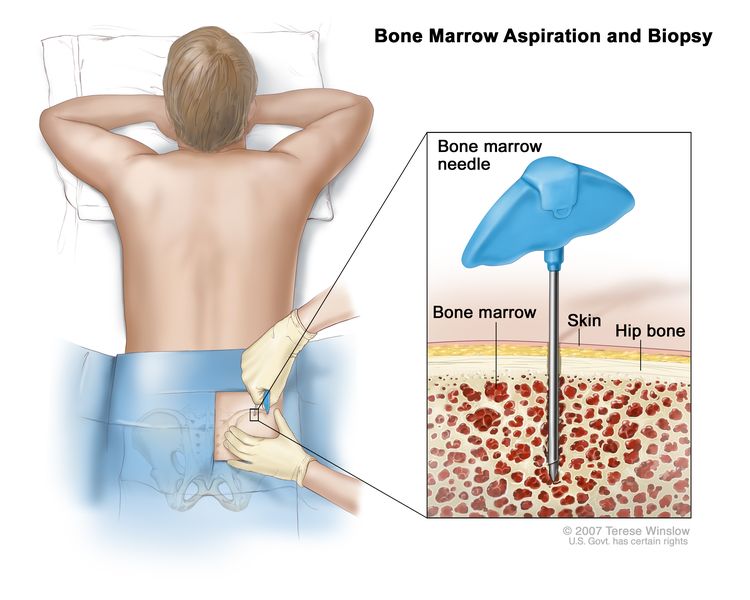
- Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for signs of cancer.
 Enlarge
Enlarge
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a bone marrow needle is inserted into the patient’s hip bone. Samples of blood, bone, and bone marrow are removed for examination under a microscope.
There is no standard staging system for primary CNS lymphoma.
Primary CNS lymphoma often recurs (comes back) after it has been treated.
Primary CNS lymphoma often recurs in the brain, spinal cord, or the eye.
Treatment Option Overview
Key Points
- There are different types of treatment for patients with primary central nervous system (CNS) lymphoma.
- The following types of treatments are used:
- Radiation therapy
- Chemotherapy
- Steroid therapy
- Targeted therapy
- High-dose chemotherapy with stem cell transplant
- Immunotherapy
- New types of treatment are being tested in clinical trials.
- Treatment for primary CNS lymphoma may cause side effects.
- Patients may want to think about taking part in a clinical trial.
- Patients can enter clinical trials before, during, or after starting their cancer treatment.
- Follow-up tests may be needed.
There are different types of treatment for patients with primary central nervous system (CNS) lymphoma.
Different types of treatment are available for patients with primary CNS lymphoma. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Surgery is not used to treat primary CNS lymphoma.
The following types of treatments are used:
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Because primary CNS lymphoma spreads throughout the brain, external radiation therapy is given to the whole brain. This is called whole-brain radiation therapy.
High-dose radiation therapy to the brain can damage healthy tissue and cause disorders that can affect thinking, learning, problem solving, reading, writing, speech, and memory. Clinical trials have tested the use of chemotherapy alone or before radiation therapy to reduce the damage to healthy brain tissue that occurs with the use of radiation therapy.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid (intrathecal chemotherapy), an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
The way the chemotherapy is given depends on where the tumor is in the CNS or eye. Primary CNS lymphoma may be treated with systemic chemotherapy, intrathecal chemotherapy, and/or intraventricular chemotherapy, in which anticancer drugs are placed into the ventricles (fluid-filled cavities) of the brain. If primary CNS lymphoma is found in the eye, anticancer drugs are injected directly into the vitreous humor (jelly-like substance) inside the eye.
Steroid therapy
Steroids are hormones made naturally in the body. They can also be made in a laboratory and used as drugs. Glucocorticoids are steroid drugs that have an anticancer effect in lymphomas.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells.
- Monoclonal antibodies: Monoclonal antibodies are immune system proteins made in the laboratory to treat many diseases, including cancer. As a cancer treatment, these antibodies can attach to a specific target on cancer cells or other cells that may help cancer cells grow. The antibodies are able to then kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells. Rituximab and nivolumab are types of monoclonal antibodies used to treat newly diagnosed or recurrent primary CNS lymphoma.
- Tyrosine kinase inhibitors: These small-molecule drugs go through the cell membrane and work inside cancer cells to block signals that cancer cells need to grow and divide. Ibrutinib is a type of tyrosine kinase inhibitor used to treat newly diagnosed or recurrent primary CNS lymphoma.
High-dose chemotherapy with stem cell transplant
High doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood-forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body's blood cells.
Immunotherapy
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer.
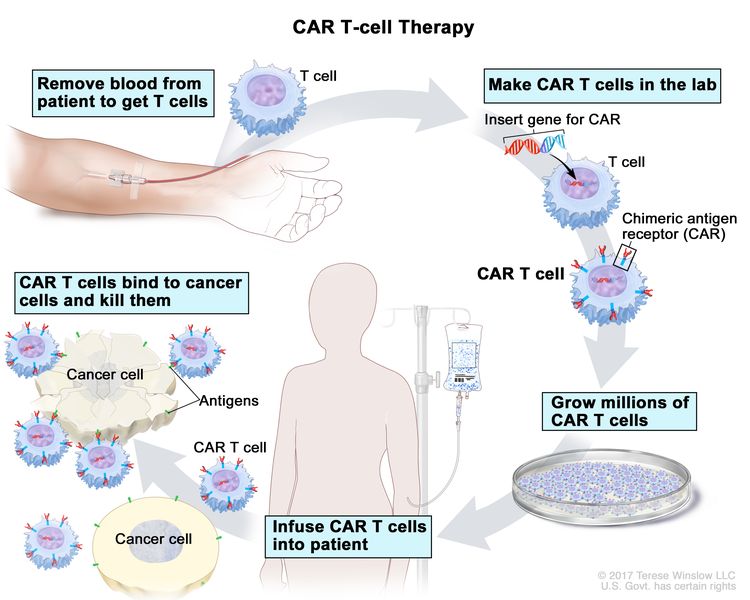
- CAR T-cell therapy: This treatment changes the patient's T cells (a type of immune system cell) so they will attack certain proteins on the surface of cancer cells. T cells are taken from the patient, and special receptors are added to their surface in the laboratory. The changed cells are called chimeric antigen receptor (CAR) T cells. The CAR T cells are grown in the laboratory and given to the patient by infusion. The CAR T cells multiply in the patient's blood and attack cancer cells.
 Enlarge
Enlarge
CAR T-cell therapy. A type of treatment in which a patient’s T cells (a type of immune cell) are changed in the laboratory so they will bind to cancer cells and kill them. Blood from a vein in the patient’s arm flows through a tube to an apheresis machine (not shown), which removes the white blood cells, including the T cells, and sends the rest of the blood back to the patient. Then, the gene for a special receptor called a chimeric antigen receptor (CAR) is inserted into the T cells in the laboratory. Millions of the CAR T cells are grown in the laboratory and then given to the patient by infusion. The CAR T cells are able to bind to an antigen on the cancer cells and kill them.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Treatment for primary CNS lymphoma may cause side effects.
For information about side effects caused by treatment for cancer, see our Side Effects page.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of Primary CNS Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed primary central nervous system (CNS) lymphoma may include the following:
- Whole-brain radiation therapy.
- Chemotherapy with or without radiation therapy.
- Targeted therapy alone (rituximab, nivolumab, or ibrutinib).
- Targeted therapy (rituximab) and chemotherapy.
- High-dose chemotherapy and stem cell transplant.
- A clinical trial of high-dose chemotherapy followed by whole-brain radiation therapy, stem cell transplant, and/or targeted therapy.
- A clinical trial of chemotherapy with or without stem cell transplant.
- A clinical trial of targeted therapy (rituximab and ibrutinib) and chemotherapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Primary CNS Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrent primary central nervous system (CNS) lymphoma may include the following:
- Chemotherapy.
- Targeted therapy (rituximab, nivolumab, or ibrutinib).
- Stem cell transplant.
- CAR T-cell therapy.
- Radiation therapy (if not received in earlier treatment).
- A clinical trial of targeted therapy (rituximab and ibrutinib) and chemotherapy.
Treatment of Primary Intraocular Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed primary intraocular lymphoma may include the following:
- Chemotherapy (intraocular or systemic) with or without radiation therapy.
- Whole-brain radiation therapy.
- Chemotherapy with targeted therapy (rituximab).
To Learn More About Primary CNS Lymphoma
For more information from the National Cancer Institute about primary central nervous system (CNS) lymphoma, see the following:
For general cancer information and other resources from the National Cancer Institute, see the following:
Updated: May 25, 2023
This content is provided by the National Cancer Institute.
Source URL: https://www.cancer.gov/types/lymphoma/patient/primary-cns-lymphoma-treatment-pdq
Make an Appointment
Your health is important. Get expert care.
Offering in-person and virtual visits.
Make an Appointment

