Clinical Rotations
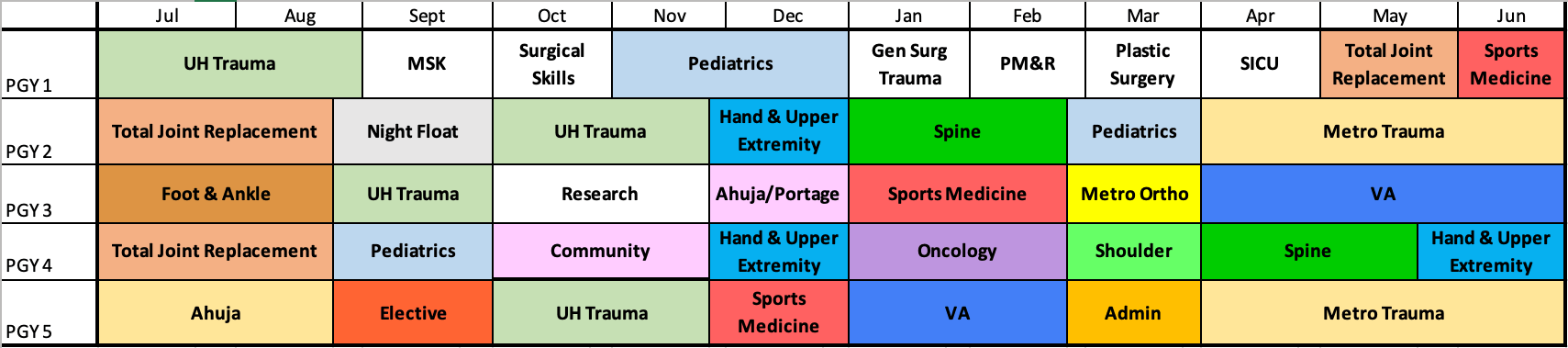
The 5 years of clinical residency consist of the PGY 1 orthopaedic surgical internship and the PGY 2-5 orthopaedic resident rotations:
The PGY-1 year consists of 12 one-month blocks, with six months of orthopaedic training and an additional one-month of basic orthopaedic education. Consistent with the ACGME’s intern-year requirements, the remaining months are rotations in non-orthopaedic fields including critical care neurosurgery, plastic surgery, physical medicine & rehabilitation, general surgery, and musculoskeletal radiology.
Years 2-5 are divided into 7-8 two-month blocks to maximize the clinical experiences and available elective time.
Basic Surgical Skills
All PGY-1 residents participate in the “Basics of Orthopaedics” Course during the month of October. During this month, all interns are free of clinical and call duty as they experience ortho “boot camp” for a month. Seminars led by faculty, staff and residents focus on the diagnosis and examination of common musculoskeletal complaints. Additionally, radiology lectures, labs for the development of psychomotor skills and the principles of internal fixation - including splinting, casting and traction techniques, the use and care of hand and power instruments, and internal fixation methods are also explored and practiced.
Multiple cadaver labs and sawbones activities are offered during this month. Fresh frozen cadavers are provided for dissection led by attending faculty focusing on common surgical approaches. In addition, basic research skills such as clinical statistics and study design are presented by the basic science faculty of the department.
Finally, this is a month of bonding for our new interns, who become a solidly integrated class during their protected time together.
Chief Elective
Chief Residents are afforded the opportunity to design portions of their rotation tailored to their own educational interests as they round out their orthopaedic surgical training during this 6 week rotation.
Chief Residents are encouraged to pursue a 1-3 week elective away rotation in pursuit of research, volunteer, or additional clinical shadowing opportunities based on the resident’s interests either domestically or internationally. These trips are funded by very generous donors who recognize the value of learning in a global setting where culture is exchanged and future relationships or networks are built.
Community Rotation/Ahuja General
Residents have the opportunity to experience community-style orthopaedics during their PGY-5 year. As the remainder of our residency is spent rotating at Level I Trauma and tertiary referral centers, this rotation allows the resident to gain exposure to a community orthopaedics practice and gain insight to practice management. The Ahuja General rotation during the PGY-4 year takes a similar approach to the chief community rotation. It allows the PGY-4 resident the opportunity to experience a community orthopaedic practice by working with attending surgeons who have a more general orthopaedic practice.
Foot & Ankle
PGY-3 Orthopedic Residents spend a dedicated block participating in the care of patients with foot and ankle conditions in the clinic and operative room. Thanks to the diverse training of the faculty, residents learn how to manage a wide variety of foot and ankle pathology, including but not limited to sports injuries, degenerative conditions, and deformity correction.
Hand & Upper Extremity
UH: Residents participate in the care of the hand and upper extremity patient as both a PGY-2 and PGY-4 resident in a predominantly outpatient focus. This rotation mainly focuses on pathology of the hand, wrist, and forearm.
Metro: Residents participate in the care of hand and upper extremity surgery patient in the elective and trauma settings. The resident will rotate on service as a PGY-4. This rotation is a combination of outpatient hand and upper extremity pathology as well as upper extremity trauma that covers all injuries from the clavicle to fingers.
MetroHealth Ortho
As a PGY-3, you spend time at Metro focusing on arthroplasty, sports medicine, spine, and foot and ankle. The PGY 3 resident takes an active role in patient care and surgical planning for primary and revision hip and knee arthroplasty. This rotation is unique as it allows for a wide breadth of exposure and is open for the PGY 3 to tailor their experience to their interest.
MetroHealth Trauma
The Metro trauma rotation occurs during both PGY-2 and Chief years. As a PGY-2 , you focus on the foundations of orthopaedic trauma and the acute management of patients with orthopaedic injuries in the emergency department as well as operative and non-operative treatment in the OR and in clinic. As a chief, your role is to help run the trauma service at Metro and take an active role in teaching junior residents in the OR, on call, and in clinic. Chiefs on the Metro rotation also work with the Trauma Fellow to plan the weekly indications conference, a resident-run conference that takes a practical approach to orthopaedic trauma education.
MSK Radiology
Residents participate in the interpretation of Musculoskeletal Imaging studies encountered during the rotation. The resident rotates with the Musculoskeletal Imaging service- as a PGY-1. This takes place primarily in the radiology reading room, but also offers the opportunity to accompany radiology faculty as they perform CT-guided biopsies in the procedure suite.
Oncology
Residents participate in the dedicated evaluation and care of orthopaedic oncology patients. The resident participates in this complex and meaningful education as a PGY-4. During this rotation, residents have the opportunity to participate in the multidisciplinary hospital-wide tumor board meeting where they assist with coordination of patient care in the setting of musculoskeletal oncology, including both metastatic disease and primary bone and soft-tissue tumors.
Pediatric Orthopaedics
Residents participate extensively in the care of pediatric orthopaedic patients. This is a balanced educational experience in line with competency-based principles of pediatric orthopaedics including, but not limited to: scoliosis, limb deformity, neuromuscular conditions, congenital malformations, sports, and trauma. Residents have exposure to outpatient clinical evaluations, inpatient consultations, and operative care, including surgical cases and technical training. Residents also participate in the weekly pediatric indications conference where they review cases with faculty and discuss high yield topics of interest.
Plastic Surgery
Residents learn the principles of correction and reconstruction of congenital and acquired defects of the head, neck, trunk and extremities, and to manage acute, chronic, and neoplastic defects not requiring complex reconstruction.
PM&R
The renowned Physical Medicine and Rehabilitation physicians at MetroHealth Hospital will help the resident become familiar with clinically applicable principles of anatomy, pathology, and biomechanics, with an emphasis on the clinical care of patients with musculoskeletal injuries and disorders. The goal of this elective rotation is to provide exposure to a broad base of physiatric learning and to encourage critical thinking, such that learners can provide compassionate care at the forefront of medical knowledge.
Research
Residents participate in a dedicated 7 week research block, which enables them to complete research in preparation for fellowship applications. The resident completes this rotation as a PGY-3.
Shoulder & Elbow
Residents participate in the care of shoulder and elbow patients with 3 fellowship trained shoulder and elbow surgeons. Residents complete this rotation as a PGY-4, participating in the management of complex patients, performing open and arthroscopic cases and arthroplasties involving the shoulder and elbow.
TICU
On this PGY-1 rotation at MetroHealth, residents learn the principles associated with the diagnosis and management of critically ill trauma patients, including simple and complex multiple organ system abnormalities, the pathophysiology of all types of shock, and the mechanisms and pathophysiology of cardiopulmonary arrest. The opportunity to learn trauma from the intensive care side helps immensely with the care of patients throughout the rest of residency. This is a favorite foundational block among our residents. While on this service interns can also take “buddy call” with the orthopaedic residents at Metro Health Medical Center.
Spine
Orthopedic residents play an active role in all aspects of the evaluation and care of patients treated by the Orthopaedic Spine division. Each resident builds and expands their knowledge of spine diseases and furthers their diagnostic, surgical, and peri-operative patient care skills during their rotation. Much growth takes place as PGY-2 and PGY-4 residents develop surgical technique using graduated autonomy from 4 excellent faculty members.
Sports Medicine
Residents participate in the care of the sports medicine patient throughout residency. The resident completes three rotations on the sports service, as a PGY-1, PGY-3, and PGY-5. During their rotation, residents gain exposure to multiple sub-specialties of orthopaedic sports medicine including shoulder and elbow, hip, and knee, developing both open and arthroscopic surgical techniques for the management of sports injuries. They can also support local sports teams and work with professional athletes.
Total Joint Replacement
Residents participate extensively in the care of the total joint patient. The resident completes three separate rotations on the total joint service, as a PGY-1, 2, and PGY-4. Residents have the opportunity to participate in clinic learning appropriate indications for total joint arthroplasty, as well as assist in the OR in a breath of total joint cases including both primary arthroplasty, learning multiple approaches to the hip, as well as complex revision cases.
Trauma
Residents spend time on trauma during their PGY-1, PGY-2, and PGY-3 years learning both operative and non-operative treatment options for orthopaedic trauma patients at UH. They spend extensive time on primary call as well as in the operating room gaining exposure to a variety of orthopaedic trauma pathologies and treatment options and growing significantly in their preoperative and intraoperative decision-making. As a PGY-5, chief residents have the opportunity to lead with a strong focus on operative management of orthopaedic injuries, as well as running daily fracture conference to take an active role in resident education.
VA
Residents participate in the care of the VAMC veterans with reconstructive, hand, and sports conditions. There are two separate rotations on the VAMC service, as a PGY-3 and again as a PGY-5. This is a great opportunity to build skills, learn autonomy, and become a much stronger diagnostic surgeon.
Call Schedule
At UH Cleveland Medical Center (Level 1 adult and pediatric trauma center), residents spend 2 months on night float as a PGY2, where they take call on weekday nights, Sunday to Thursday. Weekend call at UH Cleveland Medical Center is covered by the remaining PGY2s and PGY3s, with interns taking “buddy call” to prepare for very busy solo call nights as a PGY2. Residents rotating at MetroHealth Medical Center or Louis Stokes Cleveland VA Medical Center are not included in the UH call pool.
At UH Ahuja Medical Center Residents have the opportunity to take home call and get a feel for call as a community level surgeon. Cases that are covered are usually more of the common bread-and-butter experiences. Ahuja call is covered by PGY 3-5 level residents.
At MetroHealth Medical Center (Level 1 adult, Level 2 pediatric trauma center), residents take call as part of a rotating system. Residents are part of this call pool for 4 months as a PGY-2 and 6 weeks as a PGY-3. PGY-2s and PGY-3s take in house call. Interns also take buddy call with a PGY-2 or PGY-3 two Saturdays per month at MetroHealth while on the PM&R and TICU rotations.
At the Louis Stokes Cleveland VA Medical Center, all call is taken as home call by the on service PGY3s.
Senior Call at all institutions, our senior residents (PGY-4, PGY-5) take exclusively home call. At the VA, Metro, and Cleveland Medical Center, our PGY-4s and chiefs come into the hospital overnight/on the weekend only for surgical cases. In very rare instances, they may also come into the hospital when the junior resident requires help for a particularly difficult clinical scenario.


