Peripheral Neuropathy
What is peripheral neuropathy?
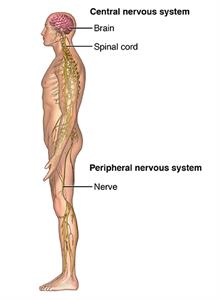
Peripheral neuropathy is a type of damage to the nervous system. Specifically, it's a problem with your peripheral nervous system. This is the network of nerves that sends information from your brain and spinal cord (central nervous system) to the rest of your body. Peripheral nerves are the nerves that exit the spinal canal or skull and go to your face, trunk, or arms and legs.
There are more than 100 types of peripheral neuropathy. Each has its own set of symptoms and prognosis. To help healthcare providers classify them, they are often broken down into these categories:
- Motor neuropathy. This is damage to the nerves that control muscles and movement in the body, such as moving your hands and arms or talking.
- Sensory neuropathy. Sensory nerves control what you feel, such as pain, temperature, or a light touch. Sensory neuropathy affects these groups of nerves.
- Autonomic nerve neuropathy. Autonomic nerves control functions that you are not conscious of, such as breathing and heartbeat. Damage to these nerves can be serious.
- Combination neuropathies. You may have a mix of 2 or 3 of these other types of neuropathies, such as a sensory-motor neuropathy.
What causes peripheral neuropathy?
Peripheral neuropathy has many different causes. Some people inherit the disorder from their parents. Others develop it because of an injury or another disorder.
In many cases, a different type of problem, such as a kidney condition or a hormone imbalance, leads to peripheral neuropathy. One of the most common causes of peripheral neuropathy in the U.S. is diabetes. Nerves can also be damaged from:
- Medicines, such as chemotherapy
- Toxins, including alcohol and some illegal drugs
- Infections like Lyme disease or HIV
Who is at risk for peripheral neuropathy?
These are risk factors for peripheral neuropathy:
- Diabetes, especially if poorly controlled
- Kidney disease
- Hormone imbalance
- Poor nutrition
- Family history of peripheral neuropathy
- Excessive alcohol use
What are the symptoms of peripheral neuropathy?
The symptoms of peripheral neuropathy vary based on the type that you have and what part of the body is affected. Symptoms can range from tingling or numbness in a certain body part to more serious effects, such as burning pain or paralysis. They may include:
- Muscle weakness
- Cramps
- Muscle twitching
- Loss of muscle and bone
- Changes in skin, hair, or nails
- Numbness
- Loss of sensation or feeling in body parts
- Loss of balance or other functions as a side effect of the loss of feeling in the legs, arms, or other body parts
- Emotional disturbances
- Sleep disruptions
- Loss of pain or sensation that can put you at risk, such as not feeling an impending heart attack or limb pain
- Inability to sweat correctly, leading to heat intolerance
- Loss of bladder control, leading to infection or incontinence
- Dizziness, lightheadedness, or fainting because of a loss of control over blood pressure
- Diarrhea, constipation, or incontinence related to nerve damage in the intestines or digestive tract
- Trouble eating or swallowing
- Life-threatening symptoms, such as trouble breathing or irregular heartbeat
The symptoms of peripheral neuropathy may look like other health problems. Always see your healthcare provider for a diagnosis.
How is peripheral neuropathy diagnosed?
The symptoms and body parts affected by peripheral neuropathy are so varied that it may be hard to make a diagnosis. If your healthcare provider suspects nerve damage, they will ask about your medical history and do a number of neurological tests. These can help determine the location and extent of your nerve damage. These may include:
- Blood tests
- Spinal fluid tests
- Muscle strength tests
- Tests of your ability to find vibrations
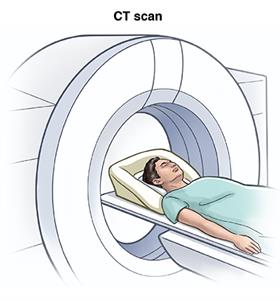
Depending on what basic tests reveal, your healthcare provider may want to do more in-depth scanning. You may need other tests to get a better look at your nerve damage, such as:
- CT scan
- MRI scan
- Electromyography (EMG) and nerve conduction studies
- Nerve and skin biopsy
- Genetic tests to diagnose neuropathies that run in families
How is peripheral neuropathy treated?
Often peripheral neuropathy can’t be cured. But you can do a lot of things to prevent it from getting worse. If an underlying condition like diabetes is at fault, your healthcare provider will treat that first. They will then treat the pain and other symptoms of neuropathy.
In some cases, over-the-counter pain relievers can help. Other times, prescription medicines are needed. Some of these medicines are:
- Mexiletine, a medicine developed to correct irregular heart rhythms
- Antiseizure medicines, such as gabapentin, phenytoin, and carbamazepine
- Some classes of antidepressants including tricyclics, such as amitriptyline
Lidocaine injections and patches may help with pain in other cases. And in extreme cases, surgery can be used to destroy nerves or fix injuries that are causing neuropathic pain and symptoms.
Physical therapy can treat weakness and muscle loss. It can also treat problems with balance. Some people may need splints or braces to help them walk.
What can I do to prevent peripheral neuropathy?
Lifestyle choices can play a role in preventing peripheral neuropathy. You can reduce your risk for many of these conditions by:
- Not drinking alcohol
- Not smoking
- Correcting vitamin deficiencies
- Eating a healthy diet
- Losing weight
- Staying away from toxins
- Exercising regularly
Living with peripheral neuropathy
Even if you already have some form of peripheral neuropathy, healthy lifestyle steps can help you feel your best. They can also reduce the pain and symptoms related to the disorder. You’ll also want to quit smoking. And don't let injuries go untreated.
Be meticulous about caring for your feet and treating wounds to prevent complications, such as the loss of a limb. Check your feet for red areas every day. Use a mirror to check between your toes and the bottoms of your feet. Contact your provider if you have an open sore.
In some cases, hand and foot braces can help you make up for muscle weakness. Orthotics can help you walk better. Relaxation methods, such as yoga, may help ease emotional as well as physical symptoms.
Key points about peripheral neuropathy
- Neuropathy affects the body in many different ways. It can affect how well you’re able to use your muscles. It can affect feeling and sensation, as well as other body functions that are automatic, such as your heartbeat.
- Medicines and lifestyle changes can improve your symptoms.
- It's important that you control any other diseases you may have to reduce your risk for peripheral neuropathy.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.