Advancing the Scope and Efficacy of Multiple Myeloma Treatments
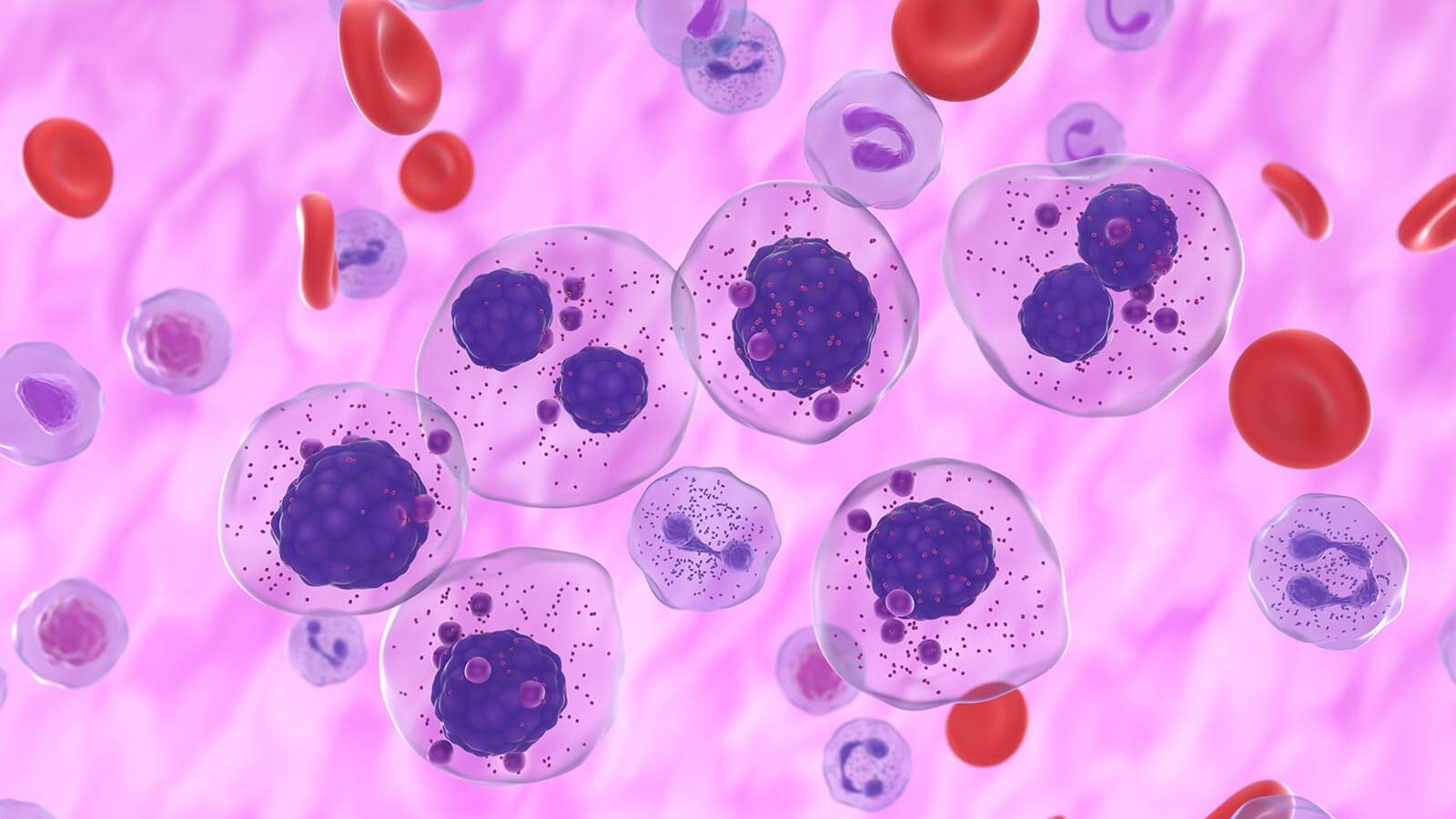
Multiple Myeloma is characterized by the excessive proliferation of clonal plasma cells, and is treatable, but incurable, although a small percentage of patients achieve long-term remission. Targeting the disease’s complex genetic heterogeneity and molecular pathophysiology via new research widens the avenue for developing new, more effective treatments.
In this growing and dynamic field, researchers are identifying novel drug targets to enhance the immune system’s ability to fight the growth of multiple myeloma cells. They are finding ways to more precisely diagnose, classify and treat individual cancers by studying the changes in genes and proteins within myeloma cells that help cancer cells grow. Such findings enable physician scientists to develop more effective therapies. They also help them assess which melanomas will grow more quickly to more accurately determine treatment strategies for individual patients.
At University Hospitals multiple myeloma researchers and clinician-scientists are developing novel next-generation therapeutics and immune therapies, including bispecific T-cell engagers (BiTEs) and onsite manufactured CAR T-cell therapy, identifying how to sequence these agents to achieve the best clinical responses, utilizing measure of residual disease.
Through continued research and collaboration our physician-scientists are identifying new immuno-oncological strategies to target multiple myeloma, improve clinical outcomes and enhance patient quality of life. They have developed multiple mixed cellular therapies to better treat multiple myeloma patients, using the most cutting-edge therapies, and drawing upon rich collaborations with pharmaceutical industries to advance standard of care.

The Wesley Center for Immunotherapy at UH Seidman Cancer Center
The Wesley Center for Immunotherapy at UH Seidman Cancer Center is a groundbreaking, state-of-the-art cellular therapy facility at the forefront of cancer care. Here, pioneering physician-scientists generate CAR T, NK cell and other cell-based therapies onsite to bring new, life-extending immunotherapy treatments more quickly to patients, without invasive leukapheresis. The Center is one of only a few nationwide to have successfully manufactured CAR T-cells for human use immunotherapy that uses the body’s own T-cells to fight cancer.


