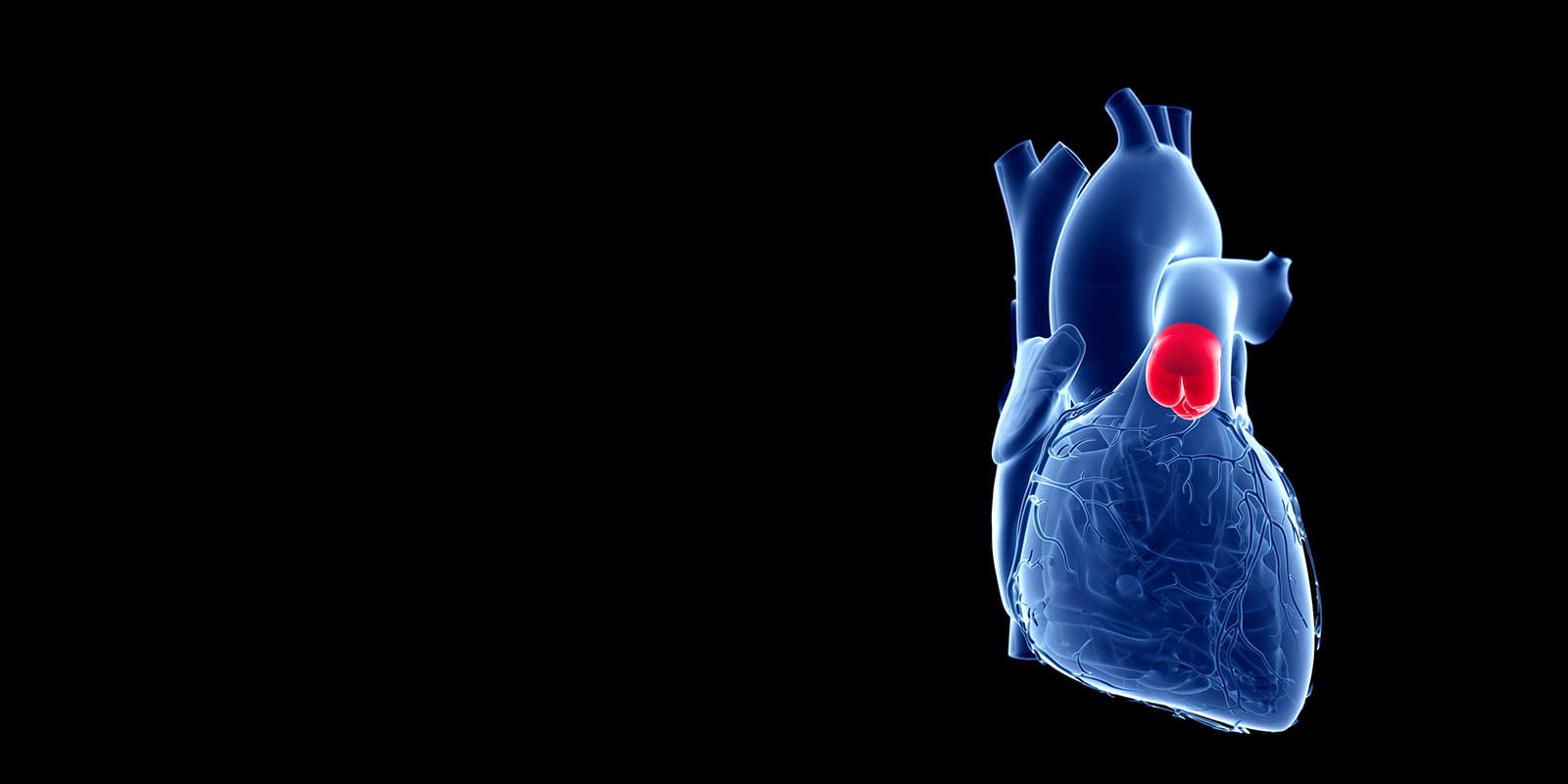
Pulmonary Valve Disease
Pulmonary valve disease is a form of heart valve disease. One of the four heart valves that keep blood flowing in the proper direction, the pulmonary valve directs blood flow from the heat’s right lower chamber (right ventricle) into the main pulmonary artery, which splits into two arteries so that blood from the heart can flow into the lungs. Pulmonary valve disease refers to conditions in which the pulmonary valve does not function normally.
Make an Appointment
Call 216-844-3800
Find a Heart Valve DoctorTreatments for Pulmonary Valve Disease
Pulmonary valve diseases treated at University Hospitals Harrington Heart & Vascular Institute’s Valve and Structural Heart Disease Center include:
Pulmonary Valve Stenosis
Pulmonary valve stenosis is a narrowing of the pulmonary valve that reduces blood flow from the heart to the pulmonary artery and lungs. Pulmonary stenosis is usually a congenital heart defect, meaning it is present at birth. However, while it is most often diagnosed in childhood, pulmonary stenosis may go undetected until adulthood or develop later in life as a symptom of another condition.
Rarely, some adults develop pulmonary stenosis later in life. Risk factors for adult (non-congenital) pulmonary stenosis include:
- Rheumatic fever, a rare complication of strep throat.
- Carcinoid syndrome, which is a set of symptoms caused by carcinoid tumors in the digestive system.
- Radiation treatment to the chest.
Symptoms of Pulmonary Stenosis
Mild pulmonary stenosis often doesn’t cause symptoms. As the narrowing increases, common heart symptoms may include:
- Chest pain
- Shortness of breath
- Fatigue, particularly growing tired easily during physical activity
- Fainting
How Is Pulmonary Stenosis Diagnosed?
Pulmonary stenosis is usually diagnosed in childhood but may not be detected or develop until later in life. When the pulmonary valve is narrowed, a doctor may hear a heart murmur during a routine examination. If pulmonary stenosis is suspected, the doctor will order additional testing, including one or more of the following echocardiography and cardiovascular imaging methods:
- Transthoracic echocardiogram (TTE)
- Electrocardiogram
- Cardiac magnetic resonance imaging (MRI)
- Cardiac catheterization
As part of the pulmonary stenosis diagnosis, your doctor will assess whether your condition is mild, moderate or severe based on the difference between the blood pressure in your right ventricle and the blood pressure in your pulmonary artery: a bigger difference in blood pressure indicates a more severe narrowing.
Pulmonary Stenosis Treatment
The experts at University Hospitals Harrington Heart & Vascular Institute’s Valve and Structural Heart Disease Center provide regular monitoring of mild and moderate pulmonary stenosis. For patients who had their pulmonary valve replaced during childhood, our adult congenital heart disease specialists and imaging experts check your prosthetic valve for signs of impaired function.
For severe cases of pulmonary stenosis, we may recommend one of the following procedures:
- Balloon valvuloplasty: A catheter-based, nonsurgical procedure in which the pulmonary valve is dilated with a balloon to repair the narrowing.
- Transcatheter pulmonary valve replacement (TPVR): A catheter-based, nonsurgical procedure for valve replacement if your previously replaced pulmonary valve is not working well enough.
- Pulmonary valve repair and replacement surgery: Surgical repair and/or replacement of the pulmonary valve can help improve blood flow and reduce symptoms of pulmonary stenosis.

Pulmonary Valve Regurgitation
In pulmonary valve regurgitation (also called pulmonary regurgitation), the flaps (leaflets) of the pulmonary valve do not close tightly enough, allowing some blood to leak backward into the heart. This condition can be mild, moderate or severe. Other names for pulmonary regurgitation include pulmonic regurgitation, pulmonary insufficiency and pulmonic insufficiency.
Symptoms of Pulmonary Regurgitation
In general, pulmonary regurgitation does not cause noticeable symptoms in infants or children. As a child grows older, however, abnormal signs and symptoms may occur, including:
- Difficulty breathing and fatigue, especially during exercise
- Sensation of rapid or irregular heartbeat (palpitations)
- Fainting during exercise or other activity
- A heart murmur (an extra sound when a doctor listens to the heart with a stethoscope)
- Chest pain, such as squeezing, pressure or tightness
- Swelling of the legs or feet
- Dizziness
- Bluish discoloration of the lips and nails (cyanosis)
Diagnosis of Pulmonary Regurgitation
Diagnosis of pulmonary regurgitation usually occurs after a primary care doctor detects a heart murmur and refers a child to a cardiologist. Testing used in the diagnosis of the condition may include some or all of the following:
- Pulse oximetry: A painless test used to measure the oxygen level (oxygen saturation) of the blood.
- Electrocardiogram (ECG): A test that assesses heart rhythm.
- Chest X-ray: A chest X-ray uses a very small amount of radiation to produce pictures of the inside of the chest.
- Echocardiogram: Also called an “echo” or cardiac ultrasound, this test uses sound waves to create video images of your heart in motion to evaluate valve function, anatomy and blood flow through the heart.
- Cardiac MRI: A test in which a three-dimensional picture of the heart’s arteries and veins is taken.
- Cardiac catheterization: Cardiac catheterization involves navigating a thin tube (catheter) through a blood vessel, usually entered via your groin, to an artery in the heart. Dye is injected into the catheter to make the artery easier to see in an X-ray.
Treatment for Pulmonary Regurgitation
Mild pulmonary regurgitation may not require treatment. Treatment options may include:
- Medication: Your doctor may prescribe medication to treat specific symptoms associated with pulmonary regurgitation, including medicines that remove extra water from the body or help control abnormal heart rhythms.
- Surgery: The most common surgeries for pulmonary regurgitation include:
- Pulmonary valve replacement: Removal of the diseased pulmonary valve and replacement with a new one.
- Conduit replacement: A procedure that involves placing a tube with a valve within it between the pulmonary artery and the right ventricle.
- Pulmonary valve repair and replacement surgery: Surgical repair and/or replacement of the pulmonary valve can help improve blood flow and reduce symptoms of pulmonary regurgitation.
- Transcatheter pulmonary valve replacement (TPVR): If you have a replaced pulmonary valve that no longer functions well, a cardiologist can perform this nonsurgical procedure to implant a new valve inside the faulty valve. The cardiologist inserts a catheter (a thin, flexible tube) through an artery in your groin; then, with the aid of advanced imaging, the doctor navigates the new tissue valve to your heart.
Make an Appointment
Call 216-844-3800


