Artificial Urinary Sphincter
What is an artificial urinary sphincter?
The urethral sphincter is a ring-shaped muscle that controls the flow of urine out of the bladder and into the urethra. The urethra is the tube that takes urine from your bladder and out of your body. When the urethral sphincter is closed (contracted), urine does not leave the bladder. When the urethral sphincter opens (relaxes), urine flows into the urethra. Normally the urethral sphincter stays closed until you need to pee (urinate).
An artificial urinary sphincter (AUS) is a man-made device that works like your urethral sphincter. It's used to treat stress urinary incontinence. This condition occurs when the urinary sphincter is weak and no longer works well. It causes urine leakage when you cough, sneeze, or strain.
AUS surgery is often done to treat incontinence after prostate surgery or radiation to the prostate. AUS surgery may be advised after other treatments have not worked.
How does an artificial urinary sphincter work?
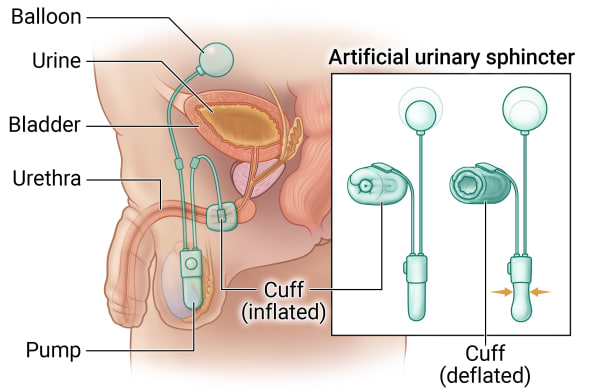
An AUS has 3 parts:
- An inflatable cuff. This ring-shaped cuff goes around your urethra. To stop urine from passing into the urethra, the cuff can be closed and inflated (filled with a sterile fluid). Urine is able to go through when the cuff is open and deflated (not filled with sterile fluid).
- A small pump. This is placed in the scrotum. It controls the flow of fluid into and out of the cuff. It's controlled by hand by squeezing the pump.
- A balloon. This is put behind your belly (abdominal) muscles. It contains the same sterile fluid as the cuff. When the cuff is open or deflated, the fluid moves into the balloon.
To pee when you have an AUS, you squeeze the pump that is in the scrotum. This moves the sterile fluid from the cuff to the balloon. The cuff then opens or deflates so that urine can pass from the bladder into the urethra. The cuff stays open for a few minutes. This allows you to pee. The cuff then closes on its own.
Why might I need an artificial urinary sphincter?
You may need AUS surgery if your urinary sphincter is not working well and you are leaking urine. This can happen after prostate surgery.
What are the risks of an artificial urinary sphincter?
All procedures have some risks. Some possible risks of this procedure include:
- Short-term bleeding
- Bruising and swelling at the insertion site, perineum, and scrotum
- Wound infection or urinary tract infection
- Inability to fully empty the bladder (urinary retention)
- A burning feeling when you pee
- Long-term (chronic) pain in your lower belly, perineum, or scrotum
- Infection or erosion of the AUS
- Problems with the AUS
- Over time, the AUS can wear out. This may happen after about 8 to 10 years. It then has to be replaced.
How do I get ready for an artificial urinary sphincter?
- Your healthcare provider will explain the procedure to you. Ask them any questions you have.
- You may need to have some tests before the surgery. This is to be sure that
you are healthy enough to have the procedure. These tests may include:
- Urine sample to be sure you don’t have a urinary tract infection
- You may be asked to sign a consent form that gives permission for the surgery. Read the form carefully and ask questions if anything is not clear.
- Tell your provider if you:
- Are sensitive to or allergic to any medicines, latex, tape, and anesthesia medicines (local and general)
- Take any medicines. This includes both over-the-counter and prescription medicines. It also includes vitamins, herbs, and other supplements.
- Have had a bleeding disorder
- Take any blood-thinning medicines (anticoagulants), aspirin, or other medicines that affect blood clotting. You may need to stop taking these medicines before the procedure.
- Make sure to:
- Stop taking certain medicines before the procedure, if advised by your provider
- Follow all directions you are given for not eating or drinking before the procedure
- Follow any other directions your provider gives you
Based on your health condition, your healthcare provider may have other instructions.
What happens during an artificial urinary sphincter?
AUS surgery often requires an overnight hospital stay. The surgery may take 2 to 3 hours. Procedures may vary depending on your condition and your healthcare provider’s practices.
Generally, AUS surgery follows this process:
- You will be asked to remove any jewelry or other objects that might get in the way during surgery.
- You will be asked to remove your clothing and will be given a gown to wear.
- An IV (intravenous) line will be put in your arm or hand.
- Before and after the surgery, you may be given antibiotics to prevent infection.
- You will be placed on an operating table.
- You will be given anesthesia. This will put you into a deep, sleep-like state for the procedure.
- A thin tube (catheter) will be placed into your bladder through the urethra. This drains urine during the surgery and for a time afterward.
- The surgeon will make a cut (incision) between your scrotum and anus (in the perineum). The cuff is placed around the urethra.
- The surgeon will make another small incision in the lower abdomen. They insert the balloon. The pump is then placed in the scrotum.
- The 3 parts of the AUS are joined using thin tubing that is filled with sterile fluid.
- The surgeon deactivates the AUS. It will be activated at a follow-up appointment about 6 weeks after surgery.
- The incisions are closed with dissolvable stitches.
What happens after an artificial urinary sphincter?
In the hospital
- After surgery, you will be taken to the recovery room to be watched. Once your blood pressure, pulse, and breathing are stable and you are awake and alert, you will be taken to your hospital room.
- The catheter may be removed before you leave the hospital. Or it may be removed at a follow-up appointment.
- It’s normal to have urine leak from your AUS after surgery. This will stop when the AUS is activated by your provider at a follow-up visit in about 6 weeks.
- Your provider will show you how to avoid activating your AUS device by mistake before your follow-up appointment. They will tell you what to do if you can’t pee.
At home
- Follow all instructions from your healthcare provider.
- You may have some pain and discomfort after the surgery and when you pee. Applying an ice pack can help. Your provider will advise you on what over-the-counter medicines to take for pain. They will give you a prescription for pain medicine if needed.
- If you go home with a catheter, it will be removed by your provider at another appointment.
- You will need to keep your wound dry for several days.
- Don’t do any heavy lifting or strenuous activity for about 4 weeks.
- Ask your provider when it is OK to drive again.
- Ask your provider when it is OK to have sex again.
- Your provider will tell you when you can go back to work and resume normal activities.
- Keep any follow-up appointments.
Call your healthcare provider if you have any of these after surgery:
- Fever
- Chills
- Redness, swelling, bleeding, or fluid leaking from the incision site
- Pain that doesn’t get better with pain medicine
- Trouble peeing
Your healthcare provider may give you other instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure


