Understanding Endometrial and Cervical Polyps
What are endometrial and cervical polyps?
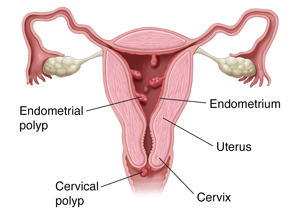
Polyps are small growths of tissue that can form in the body. If they form on the lining of the uterus (endometrium), they are called endometrial polyps. Cervical polyps grow in the cervical canal. This part of the body links the uterus to the vagina.
Most often, these types of polyps are benign (not cancer). But in rare cases, they can turn into cancer.
What causes endometrial and cervical polyps?
The exact cause of these polyps is not known. But they may occur because of changes in genes or hormones. Certain things may also raise your risk for them, such as:
- Having chronic inflammation or an infection of the cervical canal.
- Being on hormone replacement therapy.
- Taking certain medicines like tamoxifen, which helps prevent and treat breast cancer.
- Being obese.
- Having a sexually transmitted infection.
What are the symptoms of endometrial and cervical polyps?
These types of polyps often don’t cause any symptoms. If they do, you may have:
- Heavy bleeding during periods.
- Spotting, or bleeding between periods.
- Bleeding after sex.
- Pain during sex.
- Vaginal discharge or belly or pelvic pain if a polyp is infected.
How are endometrial and cervical polyps diagnosed?
Your health care provider will diagnose cervical polyps by using a speculum. This is a tool used during a pelvic exam to look at the cervix.
For endometrial polyps, your provider may use one of these tests:
- Transvaginal ultrasound
- Saline-infusion ultrasound
- Hysterosalpingogram
- Hysteroscopy
How are endometrial and cervical polyps treated?
If you don’t have any symptoms, you likely won’t need treatment. Instead, your health care provider will watch for any changes in the polyp over time. Sometimes a polyp goes away on its own.
If you have symptoms like abnormal bleeding, your provider will talk with you about removing the polyp. That’s often done with a procedure called a polypectomy. During it, your provider uses special tools to remove the polyp. This occurs during a pelvic exam.
If you are not having symptoms, your provider may still advise removing the polyp. That may be the case if:
- The polyp is large.
- You have more than one polyp.
- You are at high risk for endometrial cancer. Some things can raise your risk for this disease. These include taking tamoxifen or having gone through menopause.
What are possible complications of endometrial and cervical polyps?
Sometimes these types of polyps may come back. They may also cause problems with getting pregnant if they block the cervical canal.
When should you contact your doctor?
Contact your health care provider if you have:
- A fever of 100.4°F (38°C) or higher, or as directed by your provider.
- Symptoms that don’t get better or get worse.
- New symptoms.
Key points about endometrial and cervical polyps
-
Most often, endometrial and cervical polyps are not cancer.
-
The exact cause of these polyps is not known. But they may occur because of changes in genes or hormones.
-
If you don’t have any symptoms, you likely won’t need treatment.
-
Sometimes these types of polyps may come back. They may also cause problems with getting pregnant if they block the cervical canal.
Next steps
Tips to help you get the most from a visit to your health care provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of any new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions, especially after office hours or on weekends.


