Advanced Expertise in the Diagnosis and Treatment of Facial Paralysis
The University Hospitals Facial Paralysis Treatment Center has a team of experts with advanced training and expertise in the diagnosis and treatment of facial paralysis or dysfunction.
The facial nerve controls the muscles involved in facial expression, taste sensations and tear production. If the nerve is damaged due to injury, disease or trauma, it can result in facial paralysis, affecting the ability to speak, blink, swallow or smile. Regardless of the cause, extent or location of the nerve damage, the experts at our center can help.
Your health is important. Get expert care.
If you experience any symptoms of facial paralysis, you should immediately seek medical help. To schedule an in-person consultation with a UH facial paralysis expert, call 216-844-3223.
Virtual appointments are also available.
About Our Team
Cyrus Rabbani, MD, Director of the UH Facial Paralysis Treatment Center leads a team of ophthalmologists, oculoplastic surgeons, physical therapists and speech therapists to provide multidisciplinary, personalized treatment for each patient who comes to us for care.
Meet Our TeamDr. Rabbani explains the different types of facial paralysis and how they are treated.
What Is the Facial Nerve?
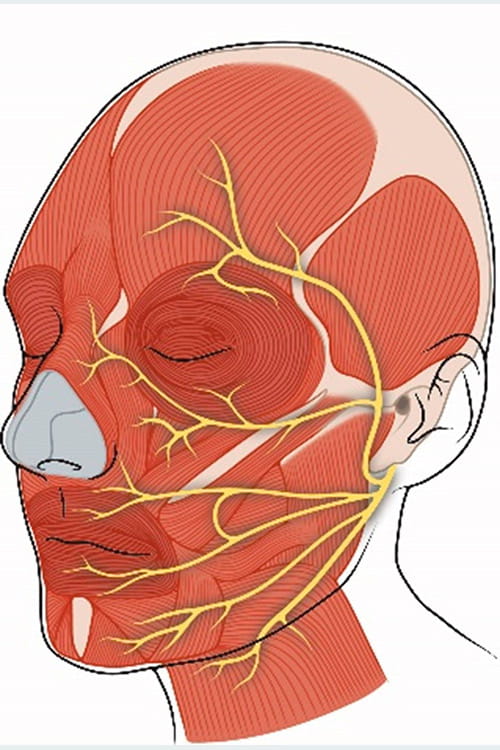
Every person has twelve cranial nerves that connect the brain to different parts of the body. The facial nerve is known as the seventh cranial nerve.
The facial nerve originates in the brain stem (base of the brain) and exits the skull through an opening located near the base of the ear and travels through the parotid gland – a salivary gland that sits just in front the ears on each side of the head. Within the parotid gland, the nerve splits into five distinct branches. Each branch exits the parotid gland and controls different areas of the face. The five branches of the facial nerve are as follows:
- Temporal or frontal: Controls the muscles of the forehead and eyebrows. When not functioning correctly, the eyebrow can droop and potentially obscure vision.
- Zygomatic: Controls the muscles around the eyelids that allow the eye to close completely. When not functioning correctly, it can cause dry eye and potentially damage the cornea if untreated.
- Buccal: Controls the muscles used to move the nostrils and upper lip. When not functioning correctly, there can be difficulties with smiling, speech, eating/drinking and spontaneous eye blinking.
- Marginal mandibular: Controls the muscles of the lower lip. When damaged, it can cause an asymmetrical smile and problems with eating and drinking.
- Cervical: Controls the lower chin muscle. Damage to this facial nerve branch may result in an asymmetrical smile.
What Causes Facial Paralysis or Dysfunction?
Facial paralysis is almost always caused by some type of damage to or deformity of the facial nerve. The damage can be present at birth (congenital) or can be caused by:
- Infections, including middle ear infections (otitis media), herpes simplex, herpes zoster (shingles) and Lyme disease.
- Traumatic injury including temporal bone fracture, birth trauma or any head injury that damages the facial nerve.
- Stroke – a stroke in the brainstem may cause long-term, debilitating facial paralysis.
- Brain tumors.
- Tumors of the inner ear (acoustic neuroma).
- Parotid gland tumors and malignancies (cancer) can invade the facial nerve.
- Surgery to remove head and neck tumors can sometimes lead to facial nerve damage.
- Ramsay Hunt Syndrome, a complication of shingles that can damage the facial nerve.
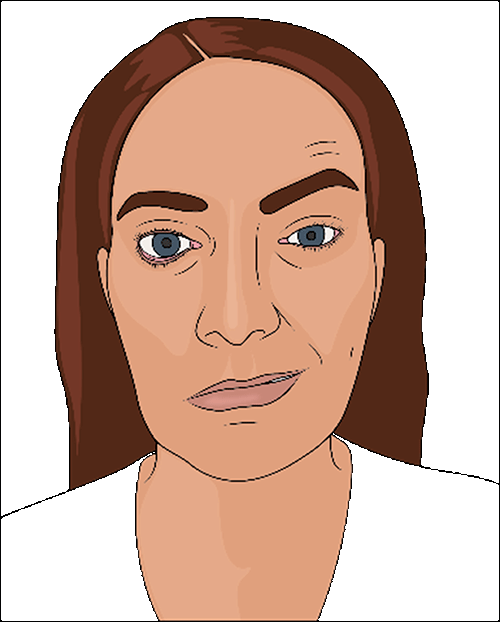
In some cases, the cause is unknown (idiopathic). The most common cause of idiopathic facial muscle weakness or paralysis is Bell’s palsy. This disorder typically has a sudden onset with symptoms worsening over the next 48 hours, and often resembling those of a stroke. This type of facial palsy usually occurs on only one side of the face, but in rare cases can affect both sides. Bell’s palsy is usually a temporary condition that resolves within three months.
Advanced Treatments for Facial Paralysis
It is very important to consult with a member of the UH Facial Paralysis Treatment Center as soon as you experience symptoms of facial paralysis to ensure the appropriate treatment is started promptly. Some conditions, such as Bell’s palsy, may resolve on their own, while others may be successfully treated with medication, physical therapy or other conservative measures. Treatments may include:
Medications
One or more of the following medications may be prescribed to help treat facial nerve inflammation and swelling:
- Antivirals. When facial nerve paralysis is caused by a virus, the symptoms are usually due to inflammation and swelling which can restrict blood flow to the facial nerve. Oral antiviral medications stop the virus from multiplying and spreading, relieve the inflammation and restore normal blood flow - allowing the nerve to heal and return to normal function.
- Corticosteroids. Steroid medications may be prescribed to reduce inflammation and swelling around the facial nerve. Usually they are taken orally for 10 to 14 days although in some cases a more aggressive approach to treatment may be required. For example, if your doctor suspects that your symptoms are causes by the herpes zoster virus (shingles), a stronger dose delivered intravenously may be the first step, followed by a course of oral medication for 7 – 10 days.
- Analgesics. If there is pain associated with your facial nerve inflammation, your doctor will recommend the appropriate pain medication(s) as part of your total treatment plan.
- Eye Drops. When facial nerve dysfunction affects the ability to blink and/or fully close the eyelid, keeping the eye lubricated is an essential part of treatment. In addition to using eye drops frequently throughout the day, your doctor may recommend the use of a lubricating gel at night, with the eye taped shut.
Injectables and Fillers
Injectables and facial fillers are often used as part of the total treatment plan for patients with facial nerve/muscle dysfunction.
They may be used separately or together to enhance facial movement, function and cosmetic appearance.
- Botulinum toxin or Botox® has been used for many years to relieve facial tightness and improve facial symmetry by weakening or paralyzing certain muscles in the face. It is most commonly used to treat tightness around the eyebrow, mouth, cheek and neck or to improve facial symmetry by weakening the muscles of the non-paralyzed side of the face. The effect is temporary, lasting approximately 3 – 6 months but can be repeated every 4 – 6 months if the results are beneficial to the patient.
- Facial fillers are used to add volume and restore symmetry to areas of the face affected by muscle atrophy. They can also be used to treat certain functional problems – for example, injecting filler around the lip can help resolve recurrent lip biting or drooling and improve certain speech problems. Facial filler treatments are typically done in the doctor’s office with local anesthesia and may last up to 18 months or more.
Rehabilitation Therapy
Many patients with facial paralysis, nerve damage or temporary facial palsy will benefit from specialized rehabilitative therapy as part of their treatment and recovery plan.
At University Hospitals, our team of physical, occupational and speech therapists carefully evaluates each patient and develops a personalized plan of care based on their diagnosis, prognosis and the severity of their condition. The goals of therapy are to:
- Stimulate, strengthen and retrain the facial nerve and supporting muscles to improve facial coordination
- Improve facial symmetry
- Regain or refine facial movements for specific functions such as speaking, eating and closing the eye
- Restore the ability to smile, frown and other facial expressions
- Correct abnormal patterns of facial movement
These goals are achieved through a series of special exercises designed to retrain the brain to coordinate the facial muscles more effectively. Our therapists take the time to teach each patient how to do the exercises properly and how often to do them for the best possible outcome.
Supplemental Procedures
To supplement other treatments, there are certain plastic surgery procedures that may be recommended as part of the total treatment plan.
Although often considered cosmetic, these surgical procedures have been shown to help relieve symptoms and improve function in certain patients with facial paralysis. These procedures include:
- Facelift
- Forehead/brow lift
- Eyelid surgery (blepharoplasty)
- Rhinoplasty
Facial Reanimation Surgery
If conservative treatments like medications and physical therapy fail to restore function and/or symmetry in patients with facial paralysis, facial reanimation surgery may be a treatment option.
Your health is important. Get expert care.
If you experience any symptoms of facial paralysis, you should immediately seek medical help. To schedule an in-person consultation with a UH facial paralysis expert, call 216-844-3223.
Virtual appointments are also available.


