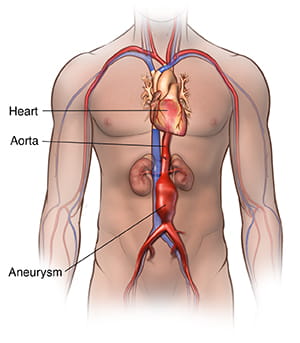
Abdominal Aortic Aneurysm
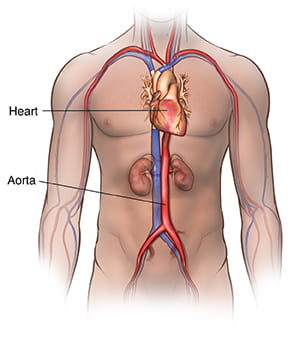
The largest blood vessel in the body, the aorta carries oxygenated blood from the heart to the rest of the body. An aortic aneurysm is a bulging, weakened area in the wall of the aorta. Aortic aneurysms occur most often in the section of the aorta that runs through the abdomen; this type of aneurysm is called an abdominal aortic aneurysm (AAA).
Treatment of abdominal aortic aneurysms is important because, over time, an abdominal aortic aneurysm can gradually grow larger and weaker, potentially bursting (a rupture) or tearing (a dissection), both of which event cause life-threatening bleeding and possibly death.
Abdominal Aortic Aneurysm Causes & Risk Factors
Several factors can contribute to the development of an abdominal aortic aneurysm, including:
- Hardening of the arteries (atherosclerosis): Atherosclerosis is a buildup of plaque in the inner lining of an artery. Plaque is a deposit of fatty substances, cholesterol, cellular waste products, calcium and fibrin.
- High blood pressure: High blood pressure can damage and weaken the walls of the aorta.
- Blood vessel diseases: Diseases that cause inflammation of blood vessels can lead to the development of an abdominal aortic aneurysm.
- Infection in the aorta: Though rare, bacterial or fungal infections can cause abdominal aortic aneurysms.
- Trauma: Traumatic injury, such as injury sustained in a car accident, can cause abdominal aortic aneurysms.
Risk factors for developing an abdominal aortic aneurysm include:
- Tobacco use: Smoking is the strongest risk factor for aortic aneurysms.
- Age: Abdominal aortic aneurysms occur most often in people age 65 and older.
- Being male: Abdominal aortic aneurysms occur in men much more often than women.
- Being white: People who are white are at higher risk of getting abdominal aortic aneurysms than non-white people.
- Family history: Having a family history of abdominal aortic aneurysms increases your risk.
- Other aneurysms: Having an aneurysm in another large blood vessel, such as the aorta in the chest (thoracic aortic aneurysm) or in the artery behind the knee, could raise your risk of developing an abdominal aortic aneurysm.
Symptoms
More often than not, abdominal aortic aneurysms do not cause noticeable symptoms. As a result, abdominal aortic aneurysms may rupture before being detected.
However, an enlarging abdominal aortic aneurysm can cause the following:
- Deep, constant pain in the belly area or side of the belly (abdomen)
- Back pain
- A pulse near the bellybutton
Symptoms of an abdominal aortic aneurysm may be similar to other conditions. Seek medical attention immediately if you suspect you have an aneurysm.
Possible Complications
The main complications of an abdominal aortic aneurysm are tears in one or more of the layers of the aorta wall (aortic dissections) or rupture. Aortic dissection and rupture are medical emergencies that can cause life-threatening internal bleeding.
Signs and symptoms of a ruptured aortic aneurysm can include:
- Sudden, intense and persistent abdominal or back pain that can be described as a tearing or ripping sensation
- Low blood pressure
- Rapid pulse
In addition, aortic aneurysms also increase the risk of developing blood clots in the area.
Abdominal Aortic Aneurysm Diagnosis
Abdominal aortic aneurysms are often discovered during a physical exam for another reason or during a routine medical test, such as an ultrasound of the abdomen or heart.
To diagnose an abdominal aortic aneurysm, your doctor will examine you and review your medical and family history. If your doctor suspects you may have an aortic aneurysm, imaging tests are done to confirm the diagnosis. These tests include:
- Abdominal ultrasound: The most common test used to diagnose abdominal aortic aneurysms, an abdominal ultrasound uses sound waves to show how blood flows through the structures in the abdominal area, including the aorta. During the test, a technician gently moves an ultrasound wand (transducer) over the skin of belly area. The device sends signals to a computer, which produces images.
- Abdominal CT scan: This imaging test captures cross-sectional images of the structures inside the abdomen using uses X-rays. An abdominal CT scan can also detect the presence, size and shape of an aortic aneurysm. During a CT scan, the patient lies on a table that slides into a doughnut-shaped machine. A dye (contrast material) may be introduced through a vein to make the blood vessels show up more clearly in the images.
- Abdominal MRI: This imaging test captures detailed images of the structures inside the abdomen using a magnetic field and computer-generated radio waves. A dye (contrast material) may be given through a vein to improve the visibility of the blood vessels.
How Are Abdominal Aortic Aneurysms Treated?
Abdominal aortic aneurysm treatment depends on the severity of the condition and if symptoms are present. Treatment options include:
- Risk Factor Management: Making some lifestyle changes may help control the progression of the aneurysm. These include quitting smoking, controlling blood sugar if you have diabetes, losing weight if you are overweight, controlling blood pressure and eating a healthy diet.
- Monitoring/Watchful Waiting with Imagining: MRI or CT tests are used to monitor an aneurysm’s size and growth rate over time.
- Medication: Your doctor may prescribe medication to control factors such as high cholesterol or high blood pressure.
- Surgery: If an aneurysm is causing symptoms or is large enough, your doctor may recommend surgery. The two main surgeries for abdominal aortic aneurysms are:
- Abdominal Aortic Aneurysm Open Repair: For this procedure, the surgeon makes a large incision in the abdomen to expose the aorta. A cylinder-like tube called a graft may be sewn to the aorta, connecting one end of the aorta at the site of the aneurysm to the other end to repair the aneurysm. Open repair is considered the surgical standard for abdominal aortic aneurysm repair.
- Endovascular Aneurysm Repair (EVAR): Requiring only small cuts in the groin, EVAR utilizes X-ray guidance and specially-designed tools to fix the aneurysm. During the procedure, the surgeon threads a graft (also called a stent graft) into the aorta and to the aneurysm from the groin incision. The stent graft is expanded inside the aorta and fastened in place to create a stable channel through which blood can flow. The stent graft reinforces the weakened part of the aorta to prevent rupture of the aneurysm. EVAR is used to treat aneurysms in the lower section of the abdominal aorta.
- Fenestrated Endovascular Repair (FEVAR): Similar to EVAR, FEVAR is used to treat aneurysms in the upper section of the abdominal aorta. Specifically, FEVAR is offered as an option for patients who are not suitable candidates for EVAR because their abdominal aortic aneurysms are too close to the arteries that branch off to the kidneys.
- Physician-modified Endovascular Grafts (PMEGs): For many patients who are anatomically unsuitable for EVAR or FEVAR, we can take standard, commercially available aortic stent grafts and customize them to the patient’s anatomy.