Alpha Thalassemia
What is alpha thalassemia?
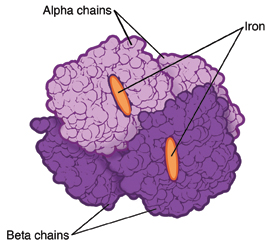
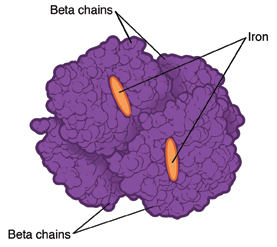
Thalassemia is a blood disorder that is inherited. This means it's passed down from one or both parents through their genes. When you have thalassemia, your body makes less hemoglobin than normal. Hemoglobin is an iron-rich protein in red blood cells. It carries oxygen to all parts of the body.
There are 2 main types of thalassemia: alpha and beta. Different genes are affected for each type.
Thalassemia can cause mild or severe anemia. Anemia occurs when your body does not have enough red blood cells or hemoglobin. The severity and type of anemia depends on how many genes are affected.
How to say it
thal-uh-SEE-mee-uh
What causes alpha thalassemia?
Alpha thalassemia occurs when 1 or more of the 4 alpha-globin genes that make up part of the hemoglobin molecule are missing or damaged.
There are 4 types of alpha thalassemia:
- Alpha thalassemia silent carrier. One gene is missing or damaged, and the other 3 are normal. Blood tests are often normal. Your red blood cells may be smaller than normal. Being a silent carrier means you don’t have signs of the disease, but you can pass the damaged gene on to your child. This is confirmed by DNA tests.
- Alpha thalassemia carrier. Two genes are missing. You may have mild anemia.
- Hemoglobin H disease. Three genes are missing. This leaves just 1 working gene. You may have moderate to severe anemia. Symptoms can worsen with fever. They can also get worse if you are exposed to certain medicines, chemicals, or infectious agents. Blood transfusions are often needed. You have a greater risk of having a child with alpha thalassemia major.
- Alpha thalassemia major. All 4 genes are missing. This causes severe anemia. In most cases, a baby with this condition will die before birth.
Who is at risk for alpha thalassemia?
This is a genetic disease inherited from one or both parents. The only risk factor is having a family history of the disease.
What are the symptoms of alpha thalassemia?
Different people will have different symptoms based on which type of alpha thalassemia is inherited. Common symptoms for each type may include:
- Alpha thalassemia silent carrier. This type has no symptoms.
- Alpha thalassemia carrier. You may have mild anemia. You may have no symptoms. Or you may have mild symptoms such as mild fatigue or trouble doing normal amounts of physical activity (exercise intolerance).
- Hemoglobin H disease. This type causes moderate to severe symptoms. These include fatigue and exercise intolerance. You may also have an enlarged liver or spleen, yellowish skin, and leg ulcers. You have a greater risk of having a child with the most severe type, alpha thalassemia major.
- Alpha thalassemia major. Babies with this type often die before they are born.
How is alpha thalassemia diagnosed?
Alpha thalassemia is most often found in these parts of the world:
- Africa
- Middle East
- India
- Southeast Asia
- Southern China
- Mediterranean region
The following blood tests are done to check for the condition and to tell if you are a carrier and can pass the disorder on to your children:
- Complete blood count (CBC). This test checks the size, number, and maturity of different blood cells in a set volume of blood.
- Hemoglobin electrophoresis. A lab test that tells what type of hemoglobin is present.
- Ferritin. This test is done to rule out iron-deficiency anemia.
- DNA testing. This test identifies which alpha-globin genes are present, absent, or damaged.
All of these tests can be done using a single blood sample. During pregnancy, the baby is diagnosed using CVS (chorionic villus sampling) or amniocentesis. A DNA test is needed to make a diagnosis of alpha thalassemia.
How is alpha thalassemia treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment may include:
- Daily doses of folic acid
- Blood transfusions (as needed)
- Surgery to remove your spleen
- Medicines to reduce extra iron from your body (called iron chelation therapy)
- Not using certain oxidant medicines in hemoglobin H disease
Living with alpha thalassemia
People with alpha thalassemia may have no symptoms. Or they may have many symptoms. If you don’t have symptoms, you may still want to see a specialist. They can help you understand the risks of passing the disease to your children.
If you have symptoms, work with your healthcare provider. They can help you find the best treatment to reduce anemia symptoms.
Key points about alpha thalassemia
- Thalassemia is an inherited blood disorder. It causes the body to make less hemoglobin than normal.
- There are 4 different types of alpha thalassemia.
- This condition causes mild to severe anemia, based on the type of alpha thalassemia that is inherited.
- People who have this condition can pass the disease on to their children.
- There is no cure. Treatment can reduce symptoms.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.


