Heart & Vascular
Showing of 208 results

UH Harrington Heart & Vascular Institute Advanced Heart Failure Director Leads New Scientific Statement on Co-Morbid Cognitive Impairment
Innovations in Cardiovascular Medicine & Surgery | Winter 2024
UH Harrington Heart & Vascular Institute Sports Cardiology Director Leads New Study of WNBA Players Published in JAMA Cardiology
Innovations in Cardiovascular Medicine & Surgery | Winter 2024

UH Harrington Heart Vascular Institute’s Chief of Cardiovascular Medicine Co-Authors Three Major Publications on Environmental Impacts in Cardiovascular Health
Recent publications lay out a roadmap and call to action - Innovations of Cardiovascular Medicine & Surgery | Winter 2024
UH Cardiac Surgeon Leads Team Generating Great Outcomes at UH Parma
UH Clinical Update | February 2024

LimFlow Technology Redefines Biology: Reverses Blood Flow to Prevent Limb Amputations
Mehdi Shishehbor, DO, MPH, PhD, explains how his team is developing preventative solutions to overcome chronic limb-threatening ischemia.
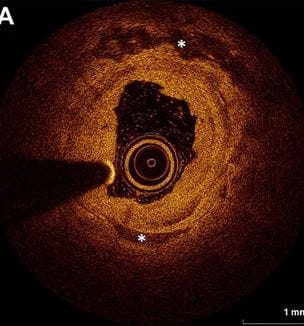
International Panel Provides Important Guidance on Treatment of Below-the-Knee Disease in Chronic Limb-Threatening Ischemia
Innovations in Cardiovascular Medicine & Surgery | February 2024

Collaboration Pushes Cardiovascular Quality to New Heights
UH Harrington Heart & Vascular Institute posts best-ever procedural outcomes - UH Harrington Heart & Vascular Update | February 2024

Groundbreaking Review of Air Pollution’s Effect on Cardiometabolic Risk Published in Lancet Diabetes Endocrinology
Innovations in Cardiovascular Medicine & Surgery | February 2024


