Monkeypox and COVID-19: Here Are Key Differences
July 26, 2022
 University Hospitals Rainbow Babies & Children'sExperts in Children's Health
University Hospitals Rainbow Babies & Children'sExperts in Children's Health
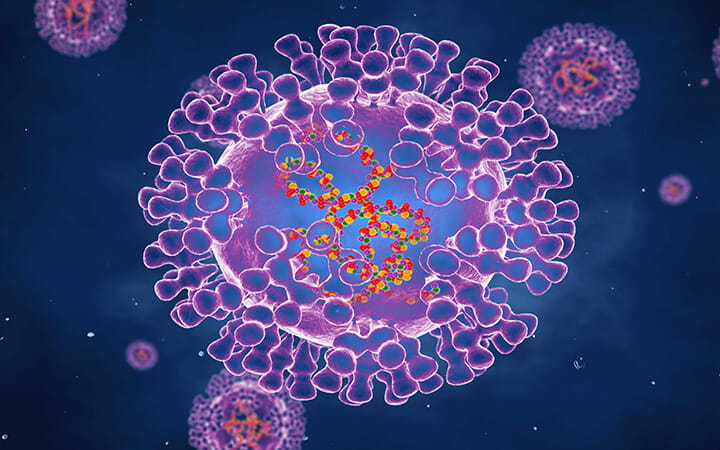
Monkeypox, a rare disease usually found in West and Central Africa, is hop-scotching across continents, with cases growing in the United States, Europe and Australia. While the outbreak is attracting headlines, there is little threat of a massive global pandemic – and no comparison to COVID-19.
There are important differences that make monkeypox a much less serious threat than COVID-19, says Amy Edwards, MD, University Hospitals Rainbow Babies & Children’s pediatric infectious disease specialist. These include:
- Monkeypox does not spread easily.
- Infected people are easier to identify.
- Outbreaks are easier to contain.
- There are two vaccines that are effective against monkeypox.
“Unlike COVID-19, this virus doesn’t transmit human to human very efficiently,” Dr. Edwards says. “It’s also much easier to isolate infected individuals and prevent the spread.”
Symptoms of monkeypox are skin rashes or lesions that spread on the body. The virus also can produce flu-like symptoms. Dr. Edwards shares more information about the virus and answers common questions.
How does monkeypox spread?
Dr. Edwards: Transmission happens during close contact – prolonged physical contact or direct contact with body fluids or lesions. It may also spread face to face through respiratory droplets or contact with contaminated bedding or clothing.
It doesn’t spread through the air like COVID-19, as far as we know. And unlike COVID-19, monkeypox isn’t contagious until the infected person becomes symptomatic. That makes it much easier to isolate infected individuals and prevent the spread.
What is the incubation period?
Dr. Edwards: The incubation is relatively long, up to one to two weeks. The smallpox vaccine or a newer smallpox/monkeypox vaccine that came out in 2019 can prevent the disease in a person who has been exposed or who is at risk of being exposed, such as a caregiver or household contact.
The fact that we already have an effective vaccine is another factor that sets monkeypox apart from COVID-19, which was a novel virus that required development of a new vaccine. We know how to handle monkeypox because it’s so closely related to smallpox.
How severe is monkeypox infection?
Dr. Edwards: Most people will have a relatively minor infection. A strain from West Africa that is spreading has a fatality rate of less than 1 percent. But that’s the mortality rate in Africa. It seems to be very different in developed countries where medical care is better.
When monkeypox jumps to another continent, it’s always the West African strain. Nobody in the United States has ever died from the West African strain. That continues to hold true during the current outbreak, though it is important to note that vulnerable populations (children, elderly and immunocompromised people) have been spared from infection so far.
There is another strain from Central Africa that is more severe. That strain is not involved in the current outbreak in North America, Europe and Australia.
Are there treatments?
Dr. Edwards: There is no specific monkeypox treatment needed for most people, but a vaccine and antiviral drugs that were developed for smallpox are effective against monkeypox.
Is there cause for alarm?
Dr. Edwards: We should take the viral outbreak as another warning that we need a strong public health sector to protect us. Right now, the monkeypox outbreak is primarily contained in adult men, who can fight the virus in most cases. If the virus jumps to large populations of children or seniors, the outlook could quickly change. The other concern is that monkeypox could jump to our rodent population and become endemic to the United States.
This outbreak shows us that our public health infrastructure isn’t sufficient. The monkeypox virus should have been manageable, but it is becoming a bigger deal every day. COVID-19 brought to light deficiencies in our underfunded public health system and now monkeypox reminds us that strong public health is our best defense.


