Executive in the Right Place at the Right Time to Receive Lifesaving Stroke Care
May 11, 2022

Eric Hess saw fireworks right before his stroke.
Fortunately, the Chief Operating Officer of University Hospitals Harrington Heart & Vascular Institute worked at UH Cleveland Medical Center – the first hospital in Northeast Ohio to achieve The Joint Commission’s rigorous standards for Comprehensive Stroke Center Certification, showcasing its ability to treat the most complex stroke cases.
Severe head and neck pain that worsened for more than a week had finally driven him to the Emergency Department. When the 52-year-old married father of three suddenly lost vision in one eye on his drive to work at main campus, and the pain had grown unbearable, he could wait no longer.
The Emergency Department staff had determined an MRI was emergently necessary to determine the source of Eric’s pain and loss of vision. An MRI is used to confirm an ischemic stroke, the type that involves a blockage in the brain and accounts for 87 percent of all strokes.
“The timing was impeccable,” said Eric. “The MRI technician told me they would be putting in the contrast, and I realized I couldn’t feel it. Within seconds, the team realized I might be having a stroke and stopped the test.”
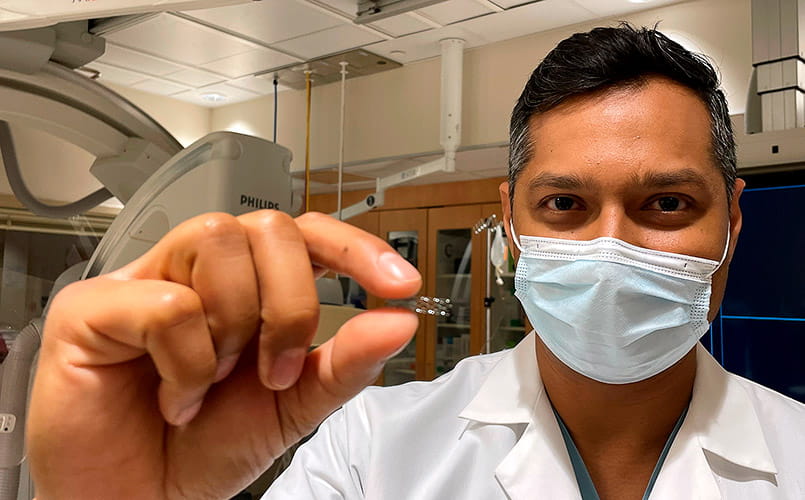
Eric also was asked to lift his left arm and leg and was unable to do so, as a large clot was blocking the majority of the right side of his brain. He was rushed off to the Interventional Radiology Lab, where neurological surgeon Abhishek Ray, MD found a challenging case beyond a common stroke.
“It was comforting, hearing these professionals discussing my condition,” said Eric, who was kept only mildly sedated in order to respond to directions from the team, as too much sedation lowers blood pressure and ample blood pressure is necessary to perfuse the blood vessels. “You’re wide awake, and they’re snaking a catheter up into your brain. I was literally hearing the team discussing the pros and cons of different stents given the nature of my dissection. As someone who has worked in the medical field for a long time, I knew I was being well cared for by professionals willing to consult with their peers to reach the best decision for optimal patient care.”
A two-front battle
Dr. Ray found Eric suffered from two complicated and acute problems simultaneously: a dissection of the inner wall of his right internal carotid artery in the neck, and a complete blockage of the middle cerebral artery that supplies the right side of the brain and controls the left side of his body.
Dr. Ray performed an intra-arterial mechanical thrombectomy, a surgical procedure to extract the 2.5 cm clot blocking blood flow to part of his brain.
“We had to remove the clot that was blocking blood flow to the right side of his brain open in order to recanalize this vessel,” said Dr. Ray. “That’s very time sensitive. The clock is ticking. Every half hour that a vessel is occluded translates to a worse outcome.”
But that was only half the battle. The section of carotid artery that was injured by dissection, a flap of the inner wall of the blood vessel, was very windy. Dr. Ray had to snake small catheters past this dissection in the carotid artery in order to place a stent and tack this flap against the vessel wall. This allowed normal blood flow to return in the carotid artery and prevent platelets from clustering and causing further strokes.
“Eric’s case was interesting, tricky and different,” Dr. Ray said. “The dissection occurred in a very tortuous and more distal part of the carotid artery, and we could not deploy the typical stents used for carotid disease in this area. I used a stent that we usually use for smaller blood vessels in the brain with a goal to get into the normal lumen of the blood vessel to tack that flap to the wall. The inner lining will remodel around the stent and heal over the next several weeks to months.”
Time is brain
When Dr. Ray extracted the clot that was obstructing blood flow to Eric’s brain, the change in his patient was immediate.
“He literally improved on the table, from not moving his left side at all to being able to lift his leg and arm,” said Dr. Ray. “There aren’t many things you do in medicine where you have that profound of a change right in front of your eyes. I find this extremely rewarding.”
Timing is critical in stroke cases. Every 40 seconds in the United States, someone suffers a stroke, and every 3.5 minutes someone dies. It’s the leading cause of long-term disability in the country.
As Dr. Ray noted, quick medical intervention could mean the difference between a person being fully paralyzed and unable to function independently to being able to walk out of the hospital and return to normal life, as Eric has done.
UH Cleveland Medical Center is the only hospital in Ohio for the second consecutive year to receive all four of the highest awards from the American Heart Association/American Stroke Association’s Get With The Guidelines®-Stroke Quality Achievement Awards. These awards were developed to help healthcare professionals provide the most up-to-date, research-based guidelines for treating stroke patients. In 2021, 14 UH hospitals earned awards for quality stroke care.
UH has been at the forefront of stroke studies and medical innovation. In 2017, through the landmark DAWN study published in the New England Journal of Medicine, the window for thrombectomy was extended to 24 hours from onset of symptoms, quadrupling the potential time for treatment. The study was led at UH by Stroke Director Cathy Sila, MD, and Dr. Ray, then completing his fellowship, recalls it as an exciting time. “We’ve had a lot of advancements in the last five to 10 years,” said Dr. Ray. “Multiple randomized studies have made intra-arterial mechanical thrombectomy standard of care for acute stroke that fits certain criteria. And with newer aspiration catheters and stent retrievers to do this procedure, we can get past windy areas that we couldn’t before and do this procedure more quickly and safely.”
Determined to work
Looking back, Eric wonders if the injury to his blood vessel occurred during an intense workout at the gym, when he was doing a lateral pulldown and afterward became lightheaded. The headaches and neck pain began after that day. But his zeal for work, and his insistence on coming in to the hospital to assist with staff appreciation rounds, delivering treats to UH Harrington Heart & Vascular Institute staff at UH Cleveland Medical Center during the holidays, may very well have saved his life.
Eric knows he was in the right place at the right time.
“My work ethic may have saved my life,” Eric said. “I knew I needed to be at the hospital. If I stayed home, I would have absolutely been dead. I would not have been found in time.”


